Translate this page into:
Burst fracture of lumbar vertebra : Aeromedicai considerations
Keywords
Burst fracture
spinal evaluation
reflighting
Spinal injuries are common during aircraft accidents. While compression fractures are commonly seen in pilots who eject from fighter aircraft equipped with ejection seats, those involved in helicopter accidents also commonly suffer from compression fractures [1]. Most frequently, such injuries affect the vertebral body. Spinal disabilities whether acquired or congenital pose significant challenges in management and decision-making. A case of burst fracture of lumbar vertebrae sustained during a helicopter accident is discussed along with the aeromedicai considerations in returning such an aircrew back to flying duties.
Case Details
A 32 year old aircrew was involved in a helicopter accident in March 2004. The pilot sustained burst fracture of second lumbar vertebra (LV2) and head injury. He also suffered post-traumatic amnesia of about 6 hours. MRI and CT brain revealed evidence of diffuse axonal injury and there were no other significant bony/soft tissue injury. CT scan of the spine revealed a stable compression fracture LV 2 with a small bony fragment protruding into the spinal canal from the posterior vertebral margins. Burst fracture of LV2 was initially managed conservatively. Later he underwent spinal fixation (Pedicle screw fixation through LV1 and LV3) for the burst fracture (Fig 1). He was subsequently managed in non flying category with implants in situ. He was observed in non-flying medical category for 48 weeks. He exhibited excellent recovery with no pain in the back during all ground activities. Evaluation of aircrew with musculoskeletal disabilities is carried out at the Department of Human Engineering, Institute of Aerospace Medicine. On complete clinical, radiological and functional recovery, the aircrew is subjected to a detailed and objective human engineering assessment. Once an aircrew has recovered with no significant deficit, he is subjected to simulated vibration stress on the vibration platform. With no demonstrable clinical, radiological or functional deficit and successful exposure to vibration stress, he was considered fit to be upgraded to a restricted flying category. He was again reviewed with an executive report on flying, including long duration sorties on helicopters. He had no complaints during flying in restricted category and was therefore upgraded to unrestricted flying category A2G2 (P). He remains asymptomatic and is pursuing an active flying career.
Discussion
Aviation stresses expose human spine to high level of forces in unique ways. These forces usually come from events such as impact and ejections. Due to unique anatomy of the thoracolumbar region [2], any excess amount of force can exaggerate forward bending property of the spine. Also any anomaly ordegenerative condition in the region has potential to alter biomechanics of spine and can predispose to spinal disability in the future [3,4]· Burst fractures are commonly seen in lumbar region as energy concentration occurs in this area due to unique regional anatomy.
Due to significant amount of forces involved in aviation, burst fractures of the vertebral body have been documented on exposure to ejection and impact forces. While wedge/compression fractures are frequently encountered in such events, burst fractures of the vertebral body are becoming much rare on account of the recent advances in crash protection systems. Burst fractures are more often seen in helicopter accidents as significant degree of vertical force [5] is involved. This has also been attributed to lack of satisfactory brace position unlike in fixed wing aircraft accidents.
Important aeromedicai issues related to burst fracture and return to flying are the effects of acceleration forces, impact forces, vibration and low backache.
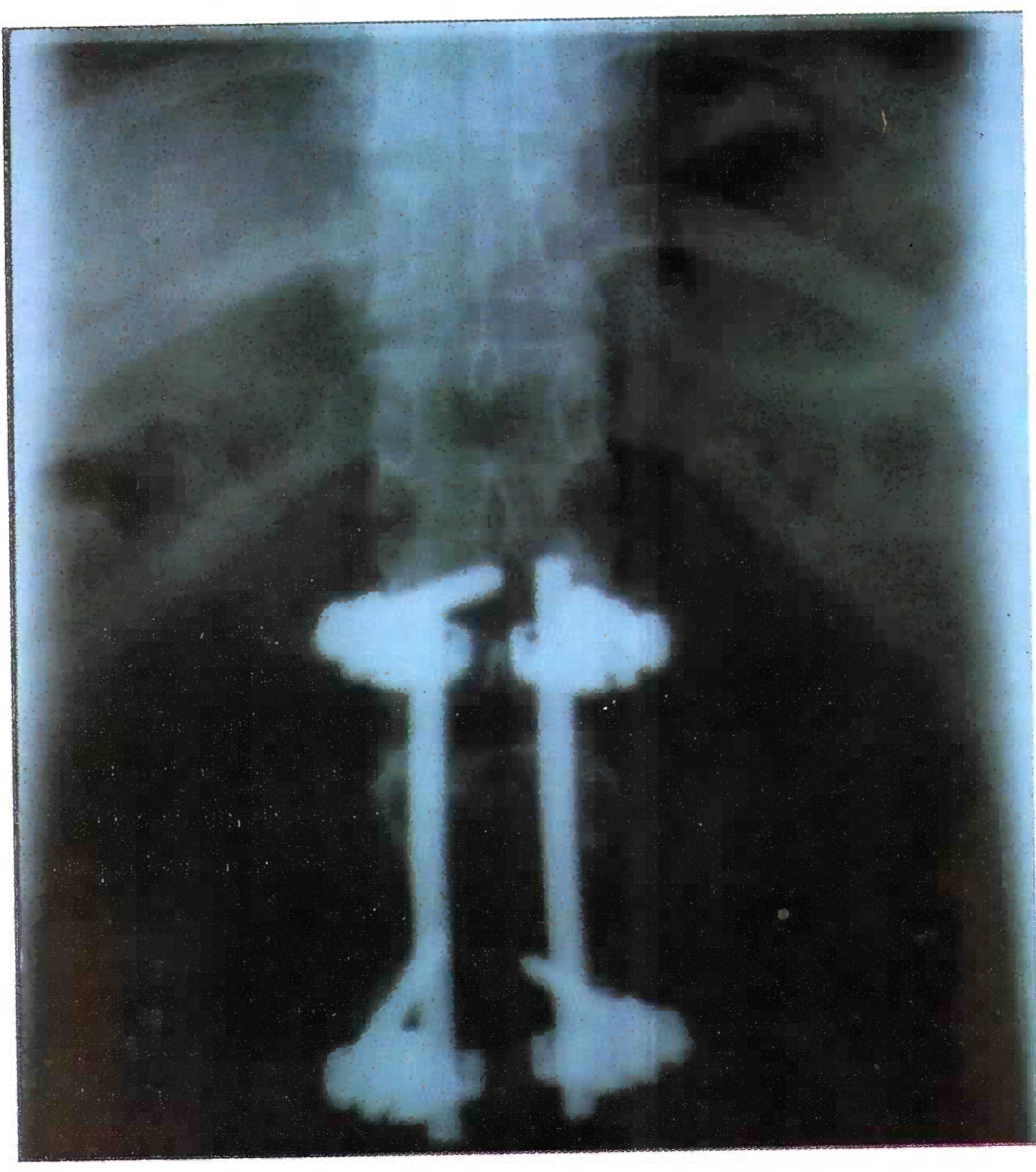
- X-ray showing implant in-situ
Burst fractures are potentially unstable. The most important factor determining neurologic recovery is the severity of the original injury. Conservative management is indicated in stable burst fractures e.g. molded turtle shell type brace (TLSO) or a body cast for 8-12 weeks. Surgical procedures are advised for unstable burst fractures only. Unstable burst fractures usually do better with early surgery. Earlier the surgery, better is the outcome in cases of unstable burst fractures. Various surgical procedures practiced include spinal fusion, laminectomy, costo-transversectomy, transpedicular resection, anterior corpectomy and plating. After any of these surgical stabilization procedures, some type of bracing is required for 8-10 weeks. Following spinal surgery, patients will remain in the hospital for 3-5 days and are usually fit with a brace once incisions have become less painful. Patients are usually allowed to walk within one or two days of surgery with the help of a physical therapist. Subsequent X-rays are taken to follow the position of the spine and degree of healing. Once the brace is discontinued, physical therapy is instituted. Most patients who do not have neurologic injury can make a near complete recovery.
Implants, which are used for spinal fixation in management of burst fracture, is another factor which poses challenges in aeromedical decisionmaking. Implants left in-situ usually pose no problems to the individual. In such cases, in si-tu metal implants may be allowed with restricted or full flying status. Rules regarding reflighting of aircrew with metal implants are not laid down; decision in such cases is done on an individual case to case basis.
Reflighting of burst fracture cases is more challenging than simple vertebral body compression fracture. This is due to the likelihood of extensive damage and instability associated with it. This is intimately related to the fine balance between conservation of trained manpower, flight safety and individual’s health; and all these aspects need to be addressed carefully. Flying status in such cases is possible in all aircraft with the exception of ejection seat aircraft, as magnitude of forces involved in fighter flying may increase severity of subsequent injury in a previously injured spine.
Rehabilitation of aircrew with burst fracture needs careful attention. Burst fracture of vertebral body may be associated with spinal cord injury. Thus detection of neurological deficit is an important part of management as injury to the spinal cord poses significant amount of morbidity. It is also an important consideration later while reflighting an aircrew with burst fracture of vertebral body. In such events there are no clear-cut guidelines laid out. Each case needs to be dealt on its merits. With the advanced management protocols available now, vertebral body burst fracture cases have better chances of full clinical and functional recovery.
Conclusion
Although burst fractures are rare, they do occur especially in rotary wing aircraft accidents. Burst fractures are potentially unstable and have propensity to cause spinal cord damage. Careful management and subsequent evaluation is very vital for follow-up of spinal injuries. With quality treatment, careful follow up and evaluation, return to flying to full flying category is possible in cases of burst fracture, thus conserving trained manpower. Decision for reflighting such cases is largely based on merits of the individual case. It presents new challenges in aeromedical decision making especially when implants are used in treatment of vertebral burst fractures.
References
- An analysis of injuries in aircrew involved in non-fatal helicopter accidents: Implications for aircrew medical examination fitness standards.
- Prevalence of vertebral compression fracture deformity by X-ray absorptiometry of lateral thoracic and lumbar spines in a population referred for bone densitometry. J Clinical Densitometry. 2002;5(3):239-46.
- [Google Scholar]
- White AA, Panjabi MM, eds. Clinical biomechanics of spine; the problem of clinical instability in the human spine - A systematic approach (2nd ed). Philadelphia: JB Lipincott Company; 1990. p. :277-378. In:
- High risk head and neck movements at high G and interventions to reduce associated neck injury. Aviat Space Environ Med. 2004;75(1):68-80.
- [Google Scholar]
- The dominance of vertebral column fractures associated with neurologic deficits among survivors of light-plane accidents. J Trauma. 1977;17(8):574-8.
- [Google Scholar]






