Translate this page into:
Analysis of G-induced Loss of Consciousness (G-LOC) and Almost Loss of Consciousness (A-LOC) incidences in high-performance human centrifuge at Institute of Aerospace Medicine Indian Air Force

*Corresponding author: Dr. A Kumar, MBBS, MD, Department of Acceleration Physiology and Spatial Orientation, Institute of Aerospace Medicine IAF, HAL Old Airport Road, Vimanapura, Bengaluru - 560 017, Karnataka, India. ajay4757giri@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar A, Nataraja MS, Sharma V. Analysis of G-induced Loss of Consciousness (G-LOC) and Almost Loss of Consciousness (A-LOC) incidences in high-performance human centrifuge at Institute of Aerospace Medicine Indian Air Force. Indian J Aerosp Med 2019;63(2):53-60.
Abstract
Introduction:
Institute of Aerospace Medicine (IAM) Indian Air Force (IAF) conducts operational training in Aerospace Medicine for IAF fighter aircrew since 2009. This includes high-G training with qualifying criteria of demonstrating ability of the aircrew to sustain 9G for 5 s in closed-loop run (pilot-in-control) wearing anti-G suit while performing anti-G straining maneuver (AGSM). Incidences of inadvertent almost loss of consciousness (A-LOC)/G-induced loss of consciousness (G-LOC) are an unavoidable unintended consequence of such training. The aim of the paper is to study the incidence of G-LOC and A-LOC and its nature in the high-performance human centrifuge (HPHC) and compare it with our previous experiences.
Material and Methods:
A G-LOC/A-LOC proforma was designed at the Department of Acceleration Physiology and Spatial Orientation at IAM IAF to understand the nature and cause of the G-LOC/A-LOC. This was to be filled up by the aircrew on a voluntary basis. The data were analyzed using Microsoft Excel with a significance level set at 95% confidence interval and alpha ≤0.05.
Results:
Fifty-two aircrew (19.92%) experienced inadvertent G-LOC/A-LOC in 83 such episodes (54 G-LOC and 29 A-LOC) during the period January 2018–December 2018. Forty-seven aircrew experiencing G-LOC/ALOC agreed to be part of the study and filled up the proforma after the episodes. The incidence of G-LOC in the institute has reduced significantly over the past two decades, perhaps due to change in the HPHC used for training of aircrew. The incidence of G-LOC found in this study is comparable to the global incidence. Rise in heart rate was higher during A-LOC than G-LOC and was found to be statistically significant (t statistic = 2.33; P = 0.01). Relative incapacitation period was lesser than absolute incapacitation period during G-LOC and was found to be statistically significant (t statistic = 3.29, P = 0.001). G-level at which Type II G-LOC occurred was significantly higher than the Type I G-LOC.
Conclusion:
The incidence of A-LOC/G-LOC has reduced over the past two decades of high G training in IAF and is comparable to global incidence.
Keywords
Human centrifuge training
Loss of consciousness
Flying
Almost loss of consciousness
G-induced loss of consciousness
INTRODUCTION
Institute of Aerospace Medicine (IAM) Indian Air Force (IAF) conducts Operational Training in Aerospace Medicine for fighter aircrew (OPTRAM-F) on a regular basis since 2009. The backbone of the course is high-G training on the high-performance human centrifuge (HPHC), installed by M/s AMST-Systemtechnik GmbH, Austria in January 2008. As a part of high-G training, aircrew is trained on L1 anti-G straining maneuver (AGSM) on the HPHC. The qualifying criterion for OPTRAM-F is to sustain 9G for 5 s by all fighter aircrew while wearing anti-G suit (AGS) and performing AGSM. The OPTRAM trainees are exposed to gradually increasing levels of G over the first 3 days of the course culminating in the qualifying run of the course, i.e., 9G for 5 s while wearing AGS and performing AGSM. All these runs are in a “closed-loop”, where the pilot pulls the control-stick to generate G-levels for the run while chasing a target aircraft which is known as target tracking (TT). This training is close to the operational scenario where aircrew may have to generate G while chasing a target during within visual range combat, missile-jinking, and dog-fight. This also concurrently tests the cognitive functions of the pilot in action as keeping the gunsight pipper on the target aircraft while pulling G and performing AGSM requires adequate cognitive functions. This makes the entire training not only physically challenging but also mentally demanding as he/she has to keep pace with his/her effort to perform adequate AGSM so that he/ she does not gray-out or black-out and loose track of the target or the weapon pointer. During this training, many aircrew experience inadvertent G-induced loss of consciousness (G-LOC)[1,2] and/or almost loss of consciousness (A-LOC or near-LOC).
G-LOC is a physiological response to sustained high G. Whinnery expanded G-LOC to G-LOC syndrome and defined it as a spectrum of neuro and psycho-physiological changes and symptoms that result from G-induced alterations in the supply of oxygenated blood to the central nervous system (CNS). It includes not only the loss of consciousness but also loss of vision, loss of muscle control, convulsive activity, dreams, altered memory, and EEG alterations.[3]
When the G stress is insufficient to cause G-LOC, deficits in motor and cognitive functions can still occur. This phenomenon is known as A-LOC. This is rather a “syndrome” with signs and symptoms of a physiological, emotional, and cognitive nature. Features of A-LOC include sensory abnormalities, amnesia, confusion, euphoria, paralysis, and reduced auditory acuity. One particularly notable feature is the apparent disconnection between the desire and the ability to perform an action. Certain features (e.g., tremor, facial twitching, and tingling) may persist for some time after the acceleration exposure is over. The underlying mechanism is thought to be similar to that of G-LOC, and it may be that a brief period of A-LOC precedes and follows G-LOC episodes.[4] The neurocognitive symptoms experienced (A-LOC) by the aircrew result in loss of situational awareness (LSA) and may lead to spatial disorientation (SD) as well. US Navy pilots have reported brief and variable episodes of confusion, amnesia, apathy, LSA, weakness, or twitching of the hands during air-combat maneuvers which are characterized by rapid onset rates (RORs) of G-loads, relatively low G levels of short duration and <1 G maneuvers.[4,5] Incidences of A-LOC during operational flying are likely to be high as it occurs at lower G-levels of shorter duration, especially if it follows negative G due to Push-Pull effect.[5,6] Even though A-LOC as a phenomenon has been reported extensively during centrifuge studies, there are very limited reports of A-LOC as a cause of an accident.[3-7] US Navy has implicated a large number of in-flight incidents of altered states of awareness to A-LOC.[4] IAF has not reported any incidence of in-flight A-LOC leading to an accident.[8] In a study spanning over a decade of centrifuge training at IAM IAF, more than 200 episodes of G-LOC in 400 pilots have been recorded. Despite the incidence of G-LOC over 30%, no incidence of A-LOC was reported in the study.[9]
IAM IAF, backed with its own experience and positive outcome of USAF, has been conducting high-G training for aircrew since March 1991 using the old centrifuge manufactured in West Germany and installed at IAM in 1966. This high G training course was initially a 5 days course and then it was changed to advance fighter aeromedical indoctrination course (AFAIC), which was of 2 weeks duration. In 2009, a new HPHC manufactured by M/s AMSTSystemtechnik GmbH, Austria, got commissioned in IAF and a 5-day comprehensive OPTRAM was introduced in place of the AFAIC. Even though centrifuge training is supervised and all efforts are made to limit pilot incapacitation due to G-LOC to a minimum, episodes of loss of consciousness do occur during such training.[1] The aim of the paper is to study the incidences of G-LOC and A-LOC and its nature in HPHC and compare it with our previous experiences.[10-12]
MATERIAL AND METHODS
The study was conducted in the Department of Acceleration Physiology and Spatial Orientation (Department of AP and SO) at IAM IAF during the period January 2018–January 2019. The Department of AP & SO houses the HPHC which can simulate the combat profile of any fighter aircraft in the world with capabilities to generate sustained +Gz acceleration up to 15G for experimental flying and 9G for human subjects at the rate up to 13 G/s instantaneous and 10 G/s sustained. It is also capable of simulating multi-axial acceleration with peak attainable values of ±6 Gy and ±10 Gx. The centrifuge has both closed-loop (pilot-in-control) and open-loop (pilot out-of-control) modes. The majority of centrifuge runs are carried out in the closed-loop mode with pilot controlled Gz onset rates and the pilot chasing a target aircraft projected on the 120° out-the-window (OTW) display. The target aircraft is pre-programmed to turn at a particular rate of +Gz. Following the target automatically exposes, the pilot to the required G level. On the contrary, the open-loop runs, where the pilot does not have any control on the +Gz onset rates, have pre-programmed rates of Gz onset and offset.
The centrifuge runs are controlled by a team of three controllers, one of whom is a physician trained in Aerospace Medicine. The aircrew undergoing the centrifuge run is under constant video monitoring. In addition, the electrocardiogram (ECG) of the aircrew is also monitored continuously. The standard operating procedure for centrifuge operations includes an immediate termination of the run by the medical controller on witnessing the aircrew eyeballs rolling up or a slumping of the head and body. In such an event, the centrifuge decelerates at a maximum offset rate of 2 Gz/s and stops.
A G-LOC/A-LOC proforma was designed in the Department of AP & SO which was to be filled on a voluntary basis by the aircrew who experienced inadvertent G-LOC/A-LOC during the OPTRAM training. Informed consent was taken before subjecting the aircrew to the questionnaire study. The G-LOC and A-LOC episodes were diagnosed by the medical operator controlling the run. The G-LOC was defined by the loss of consciousness and head slump (loss of postural control) and A-LOC was defined by stared gazed look, uprolling of the eye-balls, black-out, and manifestation of the loss of cognitive functions (e.g., stopping AGSM) without loss of consciousness. In all cases, the medical operator initiated “medical stop” at the slightest hint of aircrew slipping into inadvertent G-LOC/ALOC. The time of absolute incapacitation period (AIP) was defined as the time from dazed/blank facial expression, rolling of the aircrew’s eyeballs or sudden slumping of the head or a combination of these, to the aircrew trying to purposefully raise his head from a slumped position. The relative incapacitation period (RIP) was defined as the period from the aircrew trying to raise his head from a slumped posture to the time when he gave a definite verbal response to repeated calls from the centrifuge controller.
The aircrew undergoes HPHC training using TT run where they are controlling the onset/offset rate (max 6G/s) of the centrifuge by pulling the control-stick as they chase the target aircraft on the OTW of the gondola of the HPHC. The aircrew was instructed to start AGSM first then pull the control stick to generate G while chasing the target aircraft. The baseline HR and peak HR were noted from the HPHC run summary sheet generated at the end of every run and HR at the onset of G-LOC/A-LOC was noted from the video of the run by the medical operator.
The filled up G-LOC/A-LOC proforma received during the period of January 2018–January 2019 were analyzed using Microsoft (Excel) Office Standard 2010 version 14.0.4760.1000 (32 bit). Descriptive statistics were applied to analyze age, flying hours, time of the day, the incapacitation periods, the duration of the myoclonic flail movements, G-level at which A-LOC/G-LOC occurred and G-onset rate. Student’s t-test was used to analyze the difference between the incapacitation periods of the aircrew during A-LOC and G-LOC. Significance was set at 95% confidence interval and P < 0.05.
RESULTS
During the period of the study, 261 aircrew underwent OPTRAM training for whom 2693 runs were conducted in the HPHC. A total of 52 aircrew experienced G-LOC and/or A-LOC (20%) during this period with 54 episodes of G-LOC among 38 aircrew (2% of total runs and 15% of aircrew), 29 episodes of A-LOC among 23 aircrew (1% of total run and 9% of total aircrew) and 11 aircrew (4%) experienced both A-LOC and G-LOC.
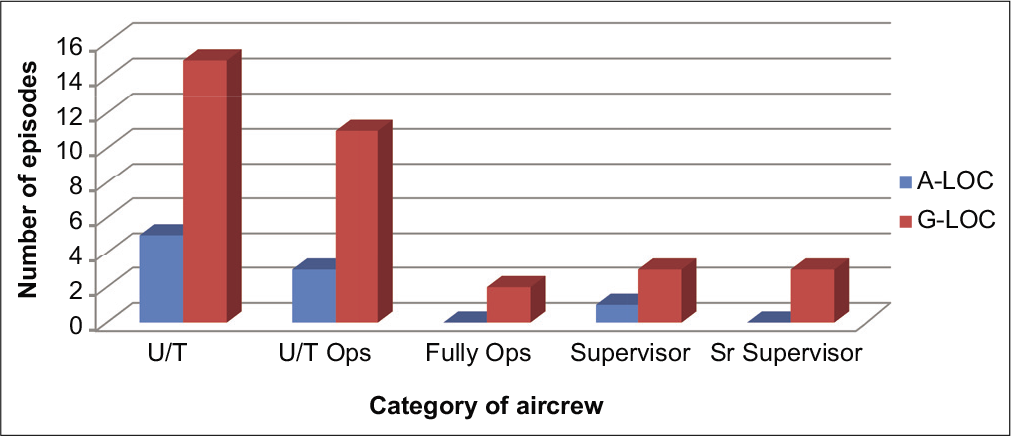
Out of the 83 episodes, a total of 47 G-LOC/A-LOC proforma were received from the respondents (57%) which consisted of 36 G-LOC episodes and 11 A-LOC episodes. The mean age of the aircrew responding to the A-LOC/G-LOC pro forma was statistically not different from the mean age of the total no of aircrew that experienced G-LOC and A-LOC during the period of the study. Rank-wise distribution of A-LOC and G-LOC proforma received is shown in Figure 1. Few columns were not filled-up in many pro forma received; however, all the proforma was analyzed. Hence, the number of samples (n) varied among many variables in the study.
- Rank-wise distribution of Almost loss of consciousness/ G-induced loss of consciousness.
The physical characteristics and relaxed gradual onset rate (GOR) tolerance of aircrew experiencing A-LOC and G-LOC were not different [Table 1]. Further, relaxed GOR tolerance of aircrew not experiencing loss of consciousness was 4.47 ± 0.6 G, which was not significantly different from relaxed GOR tolerance of aircrew experiencing A-LOC and G-LOC (P > 0.05). Distribution of A-LOC and G-LOC episodes among aircrew of various aircraft streams is shown in Table 2. There was no difference in A-LOC and G-LOC episodes as per aircraft streams.
| Parameters | A-LOC | G-LOC | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age | 25.5 | 3.3 | 26.8 | 4.9 |
| Height | 176.5 | 5.3 | 176.8 | 5.2 |
| Weight | 73.9 | 6.9 | 72.1 | 7 |
| Relaxed GOR tolerance | 4.47 | 0.69 | 4.47 | 0.54 |
GOR: Gradual onset rate, A-LOC: Almost loss of consciousness, G-LOC: G-induced loss of consciousness, SD: Standard deviation
| Aircraft flown | A-LOC (n=23) | G-LOC (n=38) |
|---|---|---|
| Basic trainer | 1 | 1 |
| Advanced jet trainer | 8 | 16 |
| Air superiority fighter | 5 | 12 |
| Non-air superiority fighter | 3 | 6 |
| Miscellaneous | 6 | 3 |
A-LOC: Almost loss of consciousness, G-LOC: G-induced loss of consciousness
Figure 1 shows the incidence of A-LOC/G-LOC as per the rank of the pilot. As expected, the incidence of A-LOC/G-LOC was highest among the trainee pilots (U/T) and lowest among the operational pilots. The incidence showed rising trend among the supervisors as a comparison to fully ops. A Chi-square analysis did not reveal any significant effect of rank on the incidence of G-LOC vis-a-vis ALOC (χ2 = 1.992, P = 0.737).
Out of 34 respondents of G-LOC proforma, eight had a history of G-LOC in the past (24%). Similarly, out of nine respondents of A-LOC proforma, three had a history of G-LOC in the past (33%). Mean duration from the last meal for the run during which A-LOC occurred was 172 min and for G-LOC, it was 179 min. Mean G-level at which A-LOC occurred was 7.5 G (SD-1.2, range 5.4–8.9 G). Similarly, mean G-level at which G-LOC occurred was also 7.5 G (SD-1.5, range 1.44–8.9 G). Mean G-onset rate for A-LOC was 3.44 ± 2.5 G/s and for G-LOC it was 2.2 ± 2 G/s. The onset rate was not significantly different between A-LOC and G-LOC (P > 0.05). The offset rate was 2G/s for all episodes as the entire run was terminated by the medical operator by pressing the “Medical Stop” button of the centrifuge.
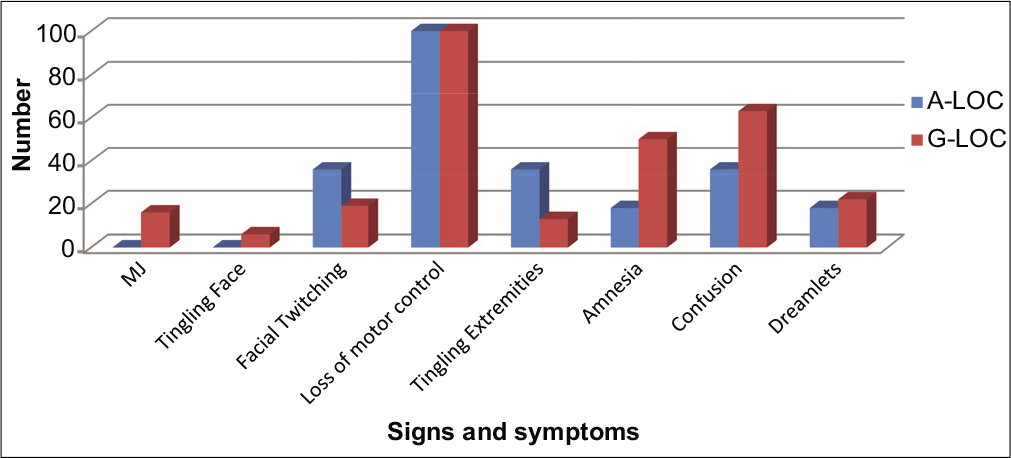
G-LOC and A-LOC syndromes [Table 3 and Figure 2] were described based on the total incapacitation period (TIP), absolute incapacitation period (AIP) and relative incapacitation period (RIP). Further, the presence of flail movement myoclonic jerks (MJ) and its duration, facial twitching, facial tingling, loss of motor control, tingling in extremities, amnesia, confusion, and dreamlets was also inquired in the proforma. The TIP for A-LOC was 10.09 ± 4.9 s and for G-LOC was 12.22 ± 4.3 s. Similarly, AIP for G-LOC was 7.29 ± 2.4 s and RIP for G-LOC was 4.92 ± 3.2 s. TIP was not significantly different between A-LOC and G-LOC (P > 0.05). However, there was a significant difference between AIP and RIP in G-LOC (t statistic - 3.29; P = 0.001).
- Details of clinical manifestation of almost loss of consciousness and G-induced loss of consciousness cases.
| Incapacitation period | A-LOC | G-LOC | ||
|---|---|---|---|---|
| Mean duration (s) | SD | Mean duration (s) | SD | |
| Relative (RIP) | - | - | 4.92 | 3.2 |
| Total (TIP) | 10.09 | 4.9 | 12.22 | 4.3 |
A-LOC: Almost loss of consciousness, G-LOC: G-induced loss of consciousness, SD: Standard deviation, RIP: Relative incapacitation period, TIP: Total incapacitation period
The A-LOC and G-LOC syndrome was studied based on their clinical manifestations, as shown in Figure 2. None of the A-LOC episodes was reported with MJ and tingling sensation on the face. About 22% of G–LOC were documented to have MJ which was of the mean duration of 3.6 ± 1.14 s (Type 2 G-LOC).
Mean basal heart, mean peak HR, and mean HR at which A-LOC and G-LOC occurred, the mean rise in HR (difference in peak HR and basal HR), the fall in HR (difference in peak HR and HR at which A-LOC/G-LOC occurred) for A-LOC and G-LOC episodes is shown in Figure 3. The rise in HR was significantly different during A-LOC and G-LOC.
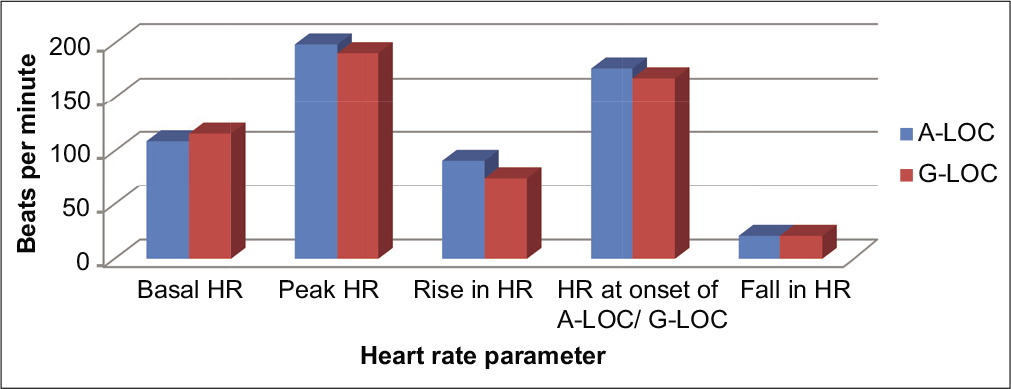
- Pattern of heart rates for almost loss of consciousness and G-induced loss of consciousness.
All respondents of A-LOC and G-LOC questionnaire reported that they were fully hydrated before the run. Two aircrew (18%) of A-LOC and five aircrew (16%) of G-LOC reported that their stomach was not full during the run. Only one aircrew (3%) reported the presence of minor ailment that was not communicated to the centrifuge operator before the run.
AGS was adequately tight during all episodes of A-LOC. AGSM was not adequate during 50% of A-LOC episodes, whereas 55% of G-LOC episodes were attributed to inadequate AGSM. Further inquiry into the inadequate AGSM performed by the aircrew who had A-LOC and G-LOC revealed various deficiencies, as shown in Figure 4.
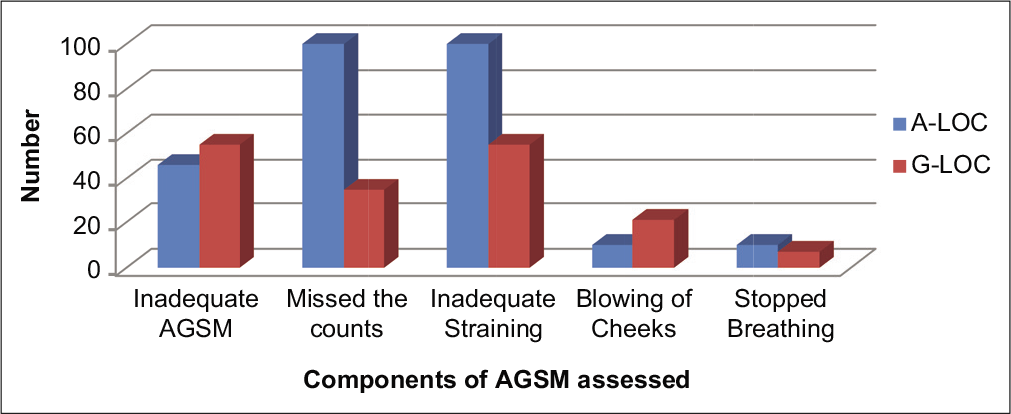
- Anti-G straining maneuver attributes during almost loss of consciousness and G-induced loss of consciousness.
Figure 5 shows the distribution of A-LOC and G-LOC episodes during various HPHC runs of the OPTRAM training. No A-LOC was reported during ROR (ROR run at 0.5 G/s), 4.5G TT, and 6G TT. The mean onset rate during closed-loop (pilot in control) runs, namely, 4.5G TT was 1G/s, 6G TT was 2G/s, 7G TT was 1.82G/s, and 9G TT was 3.16 G/s.
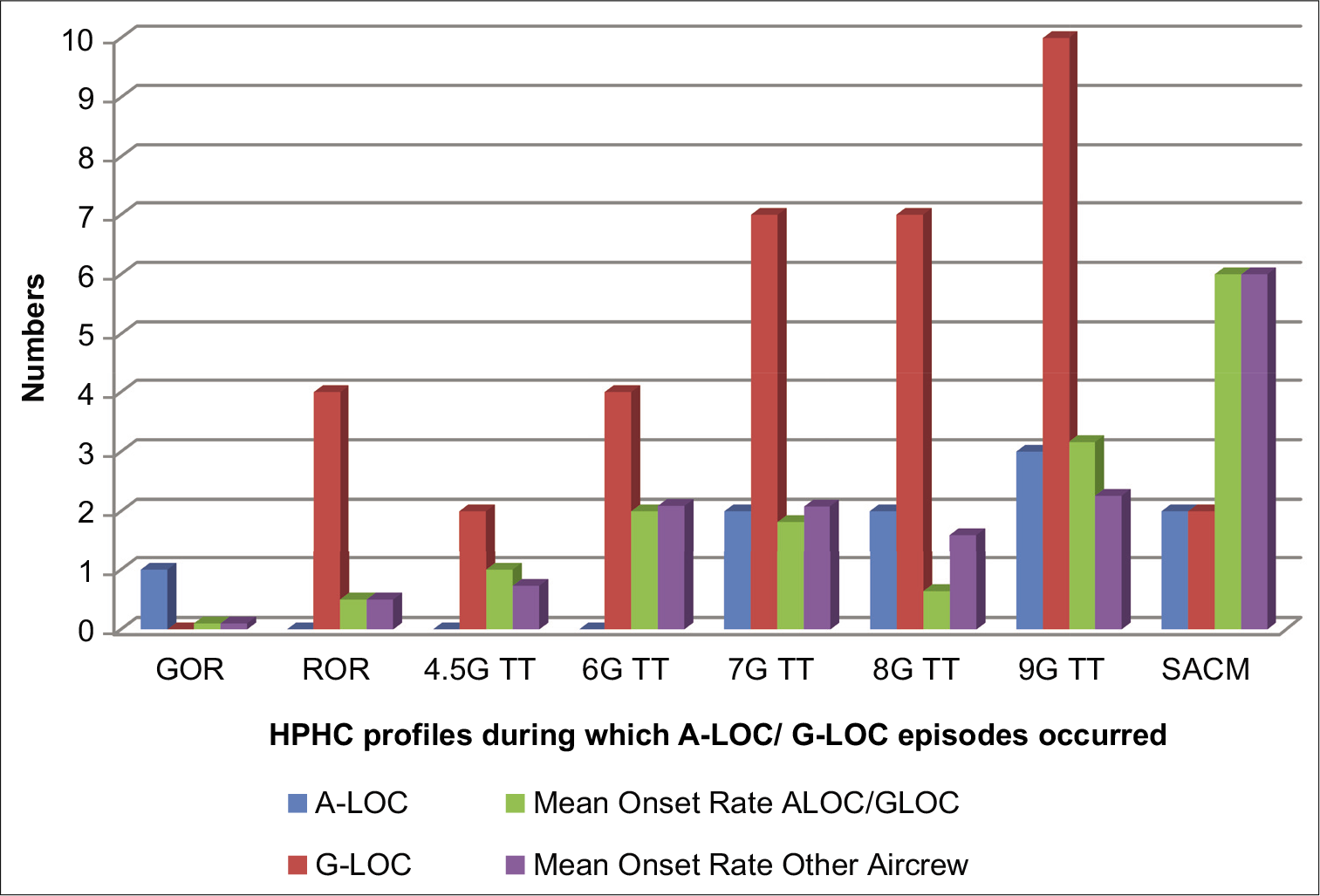
- Number of G-induced loss of consciousness and almost loss of consciousness episodes during various operational training in aerospace medicine runs.
G-LOC episodes were further analyzed to understand the difference between Type I and Type II G-LOC episodes. Total 28 Type I G-LOC (absence of myoclonic movements) and eight Type II (presence of myoclonic movements) G-LOC were reported in the A-LOC/G-LOC pro forma. Table 4 summarizes salient features of Type I and Type II G-LOC episodes.
| Parameters | P-value (T1 and T2 G-LOC) | Type I G-LOC | Type II G-LOC | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Age (years) | 0.45 | 26.07 | 4.6 | 25.88 | 4.4 | ||
| Flying hours (hours) | 559.59 | 719.90 | 604.75 | 708.50 | |||
| G-level (G) | 0.005 | 7.2 | 1.7 | 8.3 | 0.6 | ||
| G-onset rate (G/s) | 0.10 | 1.98 | 1.8 | 3.44 | 2.5 | ||
| TIP (s) | 0.30 | 12.03 | 4.8 | 12.75 | 2.5 | ||
| AIP (s) | 0.09 | 7 | 2.5 | 8.13 | 1.64 | ||
| RIP (s) | 0.38 | 5.03 | 3.5 | 4.63 | 2.6 | ||
| TIP (Modak et al.) | - | 18.40 | 5.71 | 19.75 | 6.07 | ||
| TIP Modak et al. versus present study (P) | - | <0.0001 | <0.0001 | ||||
| AIP (Modak et al.) | - | 10.88 | 4.05 | 11 | 4.76 | ||
| AIP Modak et al. versus present study (P) | - | <0.0001 | <0.0017 | ||||
| RIP (Modak et al.) | - | 7.63 | 3.98 | 8.75 | 3.75 | ||
| RIP Modak et al. versus present study (P) | - | <0.0016 | <0.0026 | ||||
| Myoclonic jerk in seconds | - | NA | NA | 3.6 | 1.1 | ||
| Basal HR (bpm) | 0.04 | 112 | 18 | 129 | 23 | ||
| Peak HR (bpm) | 0.49 | 191 | 23 | 191 | 9 | ||
| Rise in HR (bpm) | 0.09 | 79 | 27 | 62 | 26 | ||
| HR at onset of LOC (bpm) | 0.29 | 169 | 27 | 163 | 29 | ||
| Fall in HR (bpm) | 0.30 | 20 | 15 | 26 | 26 | ||
A-LOC: Almost loss of consciousness, G-LOC: G-induced loss of consciousness, SD: Standard deviation, AIP: Absolute incapacitation period, RIP: Relative incapacitation period, TIP: Total incapacitation period, HR: Heart rate
Fisher’s test was done to understand if there was any association between Type I and Type II G-LOC in the manifestation of myoclonic movements, tingling in face, twitching in face, tingling in extremities, confusion, amnesia, and dreamlets. There was no statistical association between these two groups for these manifestations (P > 0.05). Further, there was no significant difference between the state of hydration, AGS, quality of AGSM, AIP, TIP, and RIP between Type I and Type II G-LOC. There was a significant difference between AIP and RIP during Type I and Type II G-LOC. Furthermore, there was a significant difference between G-level at which Type I and Type II G-LOC were reported. There was no statistical difference in G onset rates between Type I and Type II G-LOC episodes (P > 0.05). There was no statistical difference in peak HR, rise in HR, HR at onset of LOC, and drop in HR (P > 0.05). However, the basal HR was significantly different between Type I and Type II G-LOC [Table 4].
DISCUSSION
Incidence of inadvertent A-LOC and G-LOC in HPHC during OPTRAM is an unavoidable outcome. Analysis of these episodes can reveal many facets of G-LOC/A-LOC syndromes. The incidence of loss of consciousness [Table 5] during centrifuge training has reduced significantly from previous reports; however, it is still higher than what was reported from United States Air Force (USAF).[9-13] The higher rate of loss of consciousness (almost double the incidence reported by USAF) in our study could be attributed to almost double the number of runs being given to our aircrew during the training. This explains why the 2% of total runs that resulted in loss of consciousness is comparable with the incidence reported in USAF (incidence as per total run given) and is lesser than what was reported by Agarwal et al.[12,13] The reduction in the incidence of LOC in comparison to the previous studies at the Institute can be attributed to change in training profiles and capabilities of the HPHC. The old centrifuge could not generate onset-offset rates of more than 1G/s.[7] This might have resulted in a higher incidence of G-LOC as the pilot would spend longer time in high G regime during the training as the qualifying criteria remained the same (9G for 5 s). The present training profile is more realistic where the pilot generates high-G in the course of an operational scenario where he/she is chasing the target aircraft to “lock-on” while pulling G.
| Parameter | USAF | Study I(Gomez et al.) | Study II(Agarwal et al.) | Study III(Modak et al.) | Study IV(Modak et al.) | Present study |
|---|---|---|---|---|---|---|
| Period of study | 1985–1986 | 91–94 | 91–97 | 91–2001 | 98–2001 | January–December 2018 |
| Number of subjects | 741 | 134 | 259 | 415 | 154 | 52 |
| Relaxed GOR | 5.17±0.94 | 4.97±1.03 | 4.89±0.75 | 5.01±0.7 | 5.24±0.85 | 4.5±0.6 |
| P-value (GOR compared with present study) | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | - |
| G-LOC incidence per aircrew | 9.3% | 35.8% | 35.5% | 34.69% | 33.77% | 14.56% |
| G-LOC incidence per run | 1.8% | - | 2.8% | 1.6% | - | 2% |
| ROR tolerance with AGS and AGSM | - | 8.61±0.67 | 8.73 | 8.87 | 8.87 | 7.4±1.5 |
| P-value (ROR compared with present study) | - | <0.0001 | <0.0001 | <0.0001 | <0.0001 | - |
| Age | - | 26.91 (P>0.50) | 23 (P=0.0003) | 25.7 (P>0.05) | 25.7 (P>0.05) | 26.3 |
| Height | - | 173.7 (P<0.0001) | 173.7 (P<0.0001) | 173.67 (P<0.0001) | 173.67 (P<0.0001) | 176.7 |
| Weight | - | 65.69 (P<0.0001) | 56.8 (P<0.001) | 66.26 (P<0.0001) | 66.26 (P<0.0001) | 72.8 |
| Flying experience | - | 883.40 | 795 | 600 | 600 | 549.16 |
| Course duration (days) | 1 | 6 | 6 | 12 | 12 | 5 |
| No of runs per aircrew | 5 | 30.5 | 30.5 | 30.5 | 30.5 | 10 |
| SACM AIP | - | - | - | - | 11±3.76 | 7.5±3.5 (P=0.3949) |
| SACM RIP | - | - | - | - | 12±4.24 | 2±1.4 (P=0.0635) |
| SACM TIP | - | - | - | - | 23±5.04 | 9.5±4.9 (P=0.1615) |
| ROR AIP | - | - | - | - | 10±4.69 | 7.28±2.4 (P<0.0001)* |
| ROR RIP | - | - | - | - | 8±3.92 | 5.12±3.2 (P<0.0001)* |
| ROR TIP | - | - | - | - | 19.4±6.72 | 12.4±4.3 (P<0.0001)* |
USAF: United States Air Force, IAM: Institute of Aerospace Medicine, GOR: Gradual onset rate, ROR: Rapid onset rate, AGSM: Anti-G straining maneuver, AGS: Anti-G suit, G-LOC: G-induced loss of consciousness, AIP: Absolute incapacitation period, RIP: Relative incapacitation period, TIP: Total incapacitation period. *statistically significant
The basic premise of high-G training is that onset rates affect the G-tolerance adversely. G-onset rates faster than 1 G/s (e.g., 6 G/s) result in a relaxed G tolerance approximately 0.3 G lower than the ROR tolerance thereby defining another relaxed G level tolerance called very ROR.[12,14,15] Due to this, the incidence of G-LOC and A-LOC are likely to be higher in highly agile and supermaneuverable aircraft. The reported incidence of in-flight G-LOC by USAF is 24% and Brazilian Air Force is 22%.[13] A questionnaire survey in IAF revealed in-flight G-LOC incidence to be 10.8%.[11] However, taking into consideration the associated amnesia during G-LOC, seen in approximately 50% of G-LOC episodes, the estimated in-flight incidence of G-LOC in IAF would be comparable to our study. The mean G-onset rate for A-LOC was 2.7 ± 2.1 G/s and for G-LOC, it was 2.1 ± 1.9 G/s which were not significantly different between the two groups. It implies that our pilots who experienced A-LOC and G-LOC pulled at slower onset rates from expected, i.e., 6G/s. Figure 5 shows how other pilots who did not experience A-LOC/G-LOC pulled during the OPTRAM course as well. These onset rates do not appear to be different from the A-LOC/G-LOC episodes and are lower than the expected rate of 6G/s.
The mean age of aircrew is similar to the previous study by Modak et al.[9] However, relaxed GOR tolerance in our study is 4.5 ± 0.6 G which is less than that reported by him (5.01 ± 0.7 G). This could be due to that differences in height and weight as aircrew in the present study is significantly taller and heavier than the subjects in the study of Modak et al. [Table 6].
The 22% (8 episodes) of G-LOC episodes had MJ and could be classified as Type II G-LOC in comparison to 33% reported in the study of Modak et al. No A-LOC episode was reported to have MJ which is in contrast to the study by Shender et al. who reported MJ in 30% of his subjects during A-LOC.[6] However, this was also not reported in the previous study by Sinha and Tyagi.[7] Although there was no significant difference in the G-onset rate, the G-level at which Type II G-LOC occurred was significantly higher than the G-Level at which Type I G-LOC occurred. This has a physiological basis as Type II is the manifestation of relatively severe physiological insult during the sudden critical reduction of CNS blood supply under high-G.[2] Table 6 compares the present study with the previous studies.[9,10,12,13] The TIP, AIP, and RIP are lower than the previous study of Modak et al. This is attributed to higher onset rates and offset rates of the existing HPHC which is supported by the observation that RIP is significantly lower than the AIP (P < 0.05) in the present study. AIP and RIP are functions of onset and offset rates and they are negatively correlated.[2]
CONCLUSION
The analysis of G-LOC and A-LOC incidents has given an insight into the very nature of these two important syndromes. The incidence of loss of consciousness has reduced over the past two decades in our Institute and is comparable with the global incidence. Further studies are recommended to understand the effects of known variables such as diet, hydration, alcohol, smoking and amount of sleep the previous night on the incidences of G-LOC and ALOC during High-G training.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- G-induced loss of consciousness: Definition, history, current status. Aviat Space Environ Med. 1988;59:2-5.
- [Google Scholar]
- A new look at the loss of consciousness experience within the U.S. Naval forces. Aviat Space Environ Med. 1988;59:6-8.
- [Google Scholar]
- “A-LOC”-almost loss of consciousness and it’s importance to fighter aviation. Aviat Space Environ Med. 1997;68:632.
- [Google Scholar]
- Acceleration-induced near-loss of consciousness: The “A-LOC” syndrome. Aviat Space Environ Med. 2003;74:1021-8.
- [Google Scholar]
- A-LOC: A closer look at its threat in fighter flying. Indian J Aerosp Med. 2004;48:17-21.
- [Google Scholar]
- G-related aircraft accidents in Indian Air Force. Aviat Space Environ Med. 2003;74:448.
- [Google Scholar]
- Centrifuge training visa-vis G-LOC incidents-an update. Indian J Aerosp Med. 2002;46:42-50.
- [Google Scholar]
- Centrifuge training of fighter aircrew. The Indian experience. Indian J Aerosp Med. 1994;38:84-8.
- [Google Scholar]
- G-induced loss of consciousness (G-LOC) in the Indian Air Force. Indian J Aerosp Med. 1992;36:1-5.
- [Google Scholar]






