Translate this page into:
An epidemiological study of stress fractures among flight cadets at Air Force Academy
Abstract
Stress fractures are common among flight cadets during training period and these fractures give rise to morbidity and loss of training hours. Some cadets with stress fractures are re-flighted while some are invalided out of service resulting in attrition and economic loss. A retrospective analysis of one hundred and thirty eight stress fractures among flight cadets between Jan 2000 and Oct 2004 was conducted from the case documents available at Air Force Hospital, Hyderabad. The incidence of stress fractures among cadets at Air Force Academy varied from 4.5% to 13.5% in the five years of study with minimum incidence in the year 2004. Incidence of stress fractures was higher in ground duty branch and female cadets as compared to flying branch trainees. Tibia was the commonest site of stress fracture in both sexes. In 56% of the cases the fracture occurred within 10 weeks of onset of training. On an average, cadets were hospitalized for 19.5 days. All but one case was managed conservatively. Stress fractures in flight cadets during training are due to sudden increase in amount and intensity of physical activity along with repeated impact due to running on hard surface, improper technique and equipment. Incidence and etiopathology of stress fractures have been discussed. Preventive measures adopted at Air Force Academy that have most likely led to reduction in the incidence of stress fractures are also discussed.
Keywords
Flight cadet
stress fracture
gender difference
military training
Stress fractures were first described by Briethaupt, a Prussian military physician in 1855. He described the clinical signs and symptoms of metatarsal fractures in military recruits after long marches, hence they are also known as ‘march fractures’ [1]. These are spontaneous fractures of a seemingly normal bone following a summation of stresses, which are singly insufficient to produce a fracture [2]. They are usually reported in young military recruits and trainees who are subjected to rigorous and excessive physical conditioning over a relatively short period of time.
The incidence of stress fractures in male US military recruits has been reported to range from 0.2 % to 4.5% [3]. The incidence among females in the same training programs was reportedly higher, ranging from 0.7 % to 9.6% in Officer cadets [3]. The incidence of stress fractures in Indian Army recruits has been reported to be 11.4% [4].
High incidence of stress fractures has a marked impact on the health of cadets and imposes a significant financial burden on the organization by increasing the length of training time, program costs and time to military readiness. There has been no study in the Indian Air Force (IAF) on the epidemiology of stress fractures among flight cadets during their training. The purpose of this study was to analyze the epidemiology of stress fractures among flight cadets at Air Force Academy (AFA).
Material and Methods
All cadets joining the IAF undergo a mandatory 24-week basic training at AFA. The cadets come from essentially three different backgrounds. Aircrew cadets come from either the National Defence Academy (NDA) or through the direct entry, commonly known as Combined Defence Services Examination (CDSE). Some cadets have previously served as airmen (i.e., non-commissioned officers) and are selected to get commissioned as officers. Physical fitness level of cadets coming from NDA is usually higher than the other groups. Occurrence of stress fractures among cadets during the period January 2000 to October 2004 was analyzed from the hospitalization documents.
Clinical findings of stress fracture in terms of age, sex, bone affected, causative factors, duration of hospitalization, method of treatment and its effect on final outcome of training were analyzed.
Chi-square test was applied for testing statistical significance where applicable. In all cases, the level of significance was set as p<0.05.
Results
A total of 138 cadets were clinically and radiologically diagnosed as cases of stress fracture during the study period, providing an overall incidence rate of 6.17%. The incidence of stress fracture in the 5 years covered under the study varied from 4.3% to 13.2%. The minimal incidence (4.5%) was observed in the year 2004. The year wise distribution of stress fractures is shown in Fig. 1. There was no difference in the occurrence of stress fractures in relation to the terms commencing in spring or monsoon.
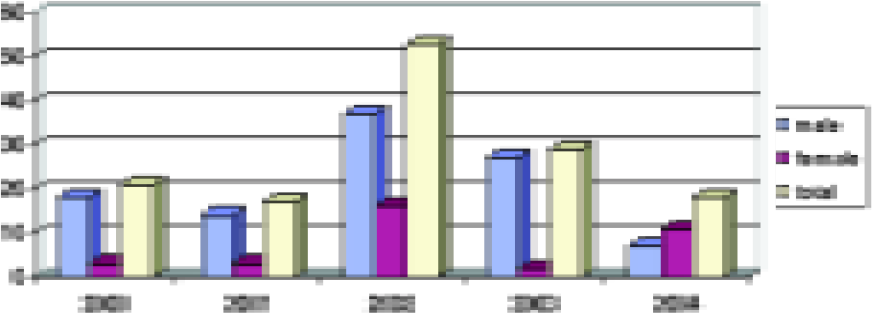
- Number of stress fractures in flight cadets
The incidence rate of stress fractures among male and female cadets was 5.8% and 7.3% respectively. These differences were not statistically significant.
The age of the cadets ranged from 20-27 years. The maximum number of stress fractures occurred in the 20 to 22 year age group. The distribution of stress fractures in relation to age is shown in Fig 2. The differences were however not significant.
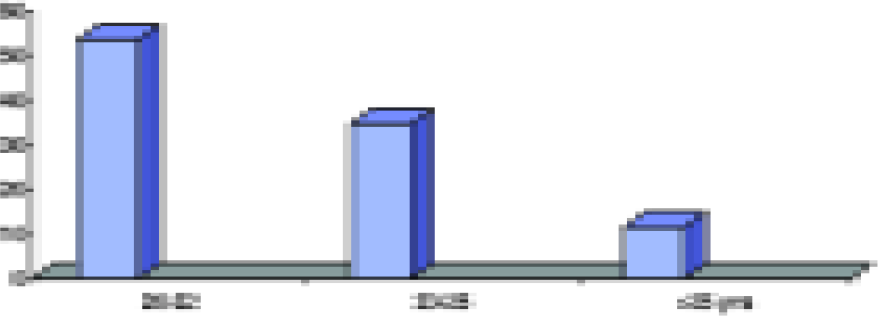
- Distribution of fractures in three age groups
94% of total stress fracture cases occurred in direct entry cadets as compared to significantly less in ex- NDA and ex- airmen as shown in Fig 3.
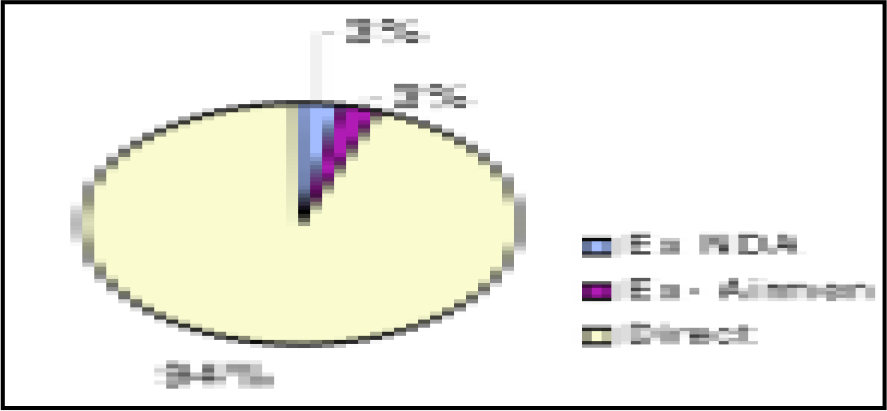
- Incidence of stress fracture in Ex-NDA, Ex-Airmen and Direct Cadets
Stress fracture of tibia was the commonest in both male (81%) and female (57%) cadets. In females, stress fracture of tibia was followed by fracture of the inferior ramus of pelvis bone in 28.5% of the cadets. The distribution of stress fractures among male and female cadets is shown in Fig 4 and 5 respectively.
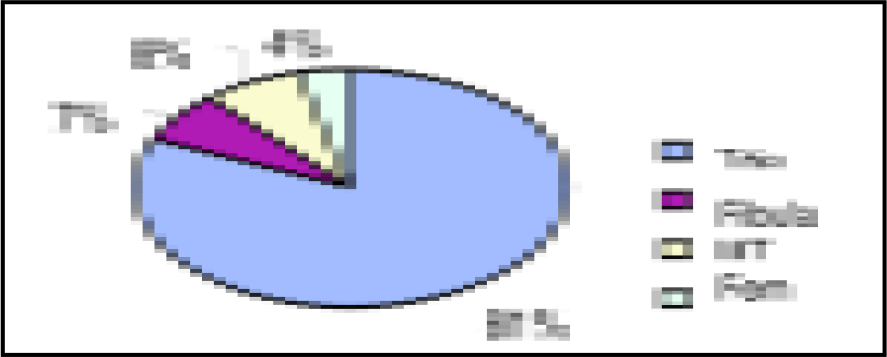
- Site distribution of stress fractures in male cadets
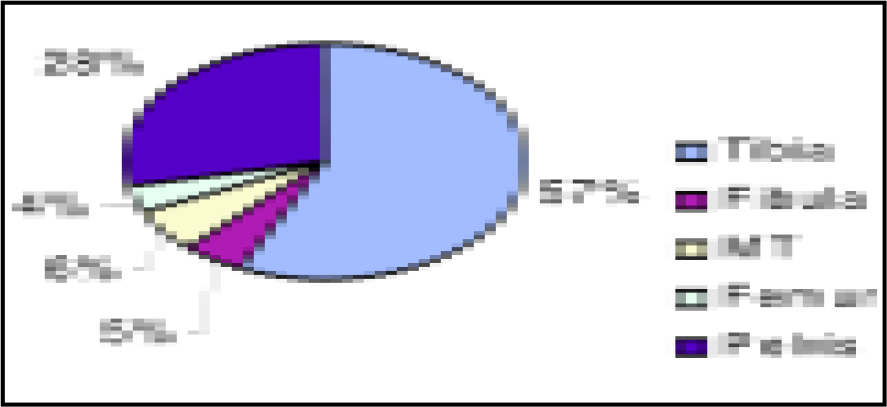
- Site distribution of stress fractures in female cadets
All cases of stress fractures were hospitalized and managed conservatively with rest and analgesics. Only one female cadet with fracture neck of femur required internal fixation. The average duration of hospitalization was 19.5 days. 76% of cadets with stress fractures completed the training successfully after recovery, 21.7% were re-flighted and 4.3% were terminated from training.
Discussion
Stress fracture is usually a hairline fracture of bone caused by rapid and repeated application of a heavy load, such as constant pounding on a surface during running, route march, parade, drill and weapon training [5]. It occurs when muscles become fatigued and are unable to absorb added shock. Eventually, the fatigued muscles transfer the overload of stress to the bone causing tiny cracks [5].
Women cadets have been reported to sustain a disproportionately higher incidence of stress fractures than men. The relative risk of stress fracture among women in military populations undergoing identical training programs as their male counterparts has been reported to be as high as 10 times [6]. However the present study did not find any significant gender based differences in the incidence of stress fractures.
The significant higher incidence of stress fractures among direct entry cadets appears to be partly due to the initial entry level of fitness and specifically the ability of bone to withstand the rapid, large increase in the intensity, frequency, or volume of impact of physical loading activities in basic training for which they were not accustomed as compared to ex- NDA and ex-airmen cadets.
In a study by Matheson et al., 95% of stress fractures involved the lower extremities with fracture of the tibia accounting for 49.1% of the fractures. This was followed by tarsal (25.3%) and metatarsal bones (8.8%), femur (7.2%), fibula (6.6%), pelvis (1.6%) and back (0.6%) [7]. Other studies have also documented tibia to be the most common bone involved in stress fractures [4,8].
The results of the present study corroborate these reported findings. Stress concentration during physical loading on tibia while running, jumping and parade on hard ground is due to its narrow and triangular shape. It is also not adequately supported by muscle mass contributing to the stress fracture.
Increased stride length during parade and running and also less muscle and bone mass as compared with same age group male trainees have been postulated to account for the increased and different site distribution of stress fractures in women cadets [4,9].
It was observed that 56% of the fractures occurred within first ten weeks of commencement of training with maximum number occurring in the eighth week. Drill with military shoes and repeated heavy stamping on hard surface or cross country running on hard, uneven surface were the immediate cause for onset of symptoms during this period of training and reporting sick in majority of cases.
It is essential to establish an early diagnosis and institute treatment as it has been documented that delay in treatment increases recovery period resulting in high training costs [10,11].
The clinical presentation can vary, thereby making diagnosis difficult. However, a thorough history can often differentiate stress fractures from other conditions. Typically, the cadet describes gradually progressive onset of pain with activity. Initially, the pain occurs only with activity and resolves with rest. Continuing the activity is associated with progression of pain. Without any modification of activity, the pain may become constant. At this point, the cadet may no longer be able to play through the pain and must withdraw from participation, prompting him or her to seek medical attention.
On physical examination, mild swelling may or may not be observed. The point of maximal tenderness on palpation of the affected bone is the hallmark of stress fractures. Percussion distal to the suspected fracture site causes transmission pain at the fracture site. Activities such as walking up and down the hallway, walking on toes, running in place, or hopping on the affected extremity often reproduce the patient’s symptoms [11].
Radiography is the method of choice to establish the diagnosis of stress fracture. Fracture lines, lucency, periosteal thickening or early callus in normal bone help in establishing a diagnosis of stress fracture. However, only 50% of stress fractures will be visualized on initial plain radiograph. Other imaging options include repeating the radiographs after 2-3 weeks, radionuclide bone scanning and magnetic resonance imaging or computed tomography. The technetium-99 diphosphonate 3-phase bone scan remains the “gold standard” as it is extremely sensitive for stress fracture. The bone scan reveals increased uptake by osteoblasts in new bone formation at the site as early as 6-72 hours after the injury [6].
The initial phase of management focuses on pain control with ice, non-steroidal anti-inflammatory medication, and relative rest. Ice application for 15-20 minutes four times per day serves the dual purpose of analgesia and reduction of soft tissue swelling. During periods of relative rest, the cadets may maintain aerobic conditioning by non- impact and non- weight bearing training activities which includes swimming, running with a flotation device, cycling and upper body weights.
Re-induction into scheduled military training of treated cases of stress fracture has to be gradual and methodical to avoid recurrence.
Prevention
A small number of stress fractures among trainees in any military training centre is inescapable. But the number can be kept minimal if training schedule and other parameters are modified suitably. The cornerstone in stress fracture prevention rests on education of trainees, trainers and instructors. The following preventive measures were adopted at AFA since January 2003 which helped in reduction of stress fractures. The preventive measures being practiced are :-
An integrated program designed to start with low level of activity and gradually increasing the level of activity to transition into full- scale basic training within 4-6 weeks.
Commencement of high-strain, physical training activities after approximately 6 weeks of graduated endurance training in circuit gym and yogic exercise schedule.
Training commencing on surfaces that absorb shock to the greatest extent, such as leveled soft ground, progressing to hard paved surface and finally tarred drill ground.
Curtailment of unstructured physical activity in the name of toughening by seniors and rest from all physical activities once a week allowing recuperation of musculoskeletal fatigue.
Muscle training before and after protracted physical activity.
Use of good shock absorbing, smooth tread, rocker-sole design, flexible and lightweight, well fitting activity-specific shoes.
Consumption of appropriately higher energy food matched to meet the demands of physical training and fitness.
Early diagnosis and institution of treatment to prevent further progression of injury. After discharge from hospital, the cadets are reintroduced to physical training by graded non-loading activities like cycling, swimming and yoga exercises.
Initial indoctrination and periodic education of trainees and instructors about the aetio-pathogenesis and prevention of stress related injuries.
Conclusion
The principal factor in causation of stress fracture is rigorous and sustained physical activity over a relatively short period of time in an unaccustomed cadet. The proactive approach for preventing stress fractures is to start at a lower level of activity and gradually progress to full-scale basic training. Training program should also include muscle endurance training to help the cadets withstand intense physical activity. Proper footwear and appropriate running surface also contribute to the prevention of injuries. While complete elimination of stress fractures is impractical, an objective approach to minimize loss of training hours should be the goal of all training establishments.
References
- Stress Fractures in Athletes: Risk Factors, Diagnosis, and Management. Clinical Journal of Sports Medicine. 2001;11(2):73-6.
- [Google Scholar]
- Use of simple measures of physical activity to predict stress fractures in young men undergoing a rigorous physical training program. Am J Epidemiology. 1999;149:236-42.
- [Google Scholar]
- Stress fractures: management using a new classification. Indian Journal of Orthopedics. 2004;38(2):112-20.
- [Google Scholar]
- Prevention of stress fractures in athletes. Retrieved on 26 Oct 04 from the world wide web: http://www.nap.edu
- [Google Scholar]
- Stress fractures in athletes. How to spot this underdiagnosed injury. Postgrad Med. 1991;89:185-88.
- [Google Scholar]
- Stress fractures in athletes: A study of 320 cases. Am J Sports Med. 1987;15:46-58.
- [Google Scholar]
- The incidence and distribution of stress fractures in competitive track and field athletes: A twelve-month prospective study. Am J Sports Med. 1996;24:211-17.
- [Google Scholar]
- Stress fractures: Clinical history and physical examination. Clin Sports Med. 1997;16:259-74.
- [Google Scholar]






