Translate this page into:
A retrospective analysis of injuries among aircrew involved in helicopter accidents
Abstract
Despite advancements in the crashworthiness of helicopters, both the rate and severity of injuries sustained in helicopter accidents remain a cause for concern. While various studies have documented the injuries sustained by pilots during ejections and fatal helicopter accidents, there has been no analysis of injuries in non fatal helicopter accidents. The present study was carried out to analyze injuries in aircrew involved in non fatal helicopter accidents. Medical records of a total of 52 aircrew involved in non fatal helicopter accidents during the period of study were retrieved for analysis. The mean age of the pilots was 31yrs (24-44 yrs) whereas the mean age of the non-pilot aircrew was 33.6 yrs (29 - 49 yrs). All except seven (Army =5, Navy =2) were from the Air Force. Of the 52 aircrew, there were 7 (13.5%) who did not suffer any injury. Of the 45 aircrew who suffered some form of injury, 8 had multiple injuries thus giving a total of 53 injuries. Of these, 43.4% were spinal injuries (n=23) followed by head and face (22.6%, n=12). A total of 16 aircrew sustained 28 vertebral fractures, majority of them being at the thoracolumbar region. While the pilots sustained more of spinal injuries, head and face injuries were the leading injuries sustained by the non pilot aircrew. This study provides a preliminary understanding of the nature of injuries in aircrew involved in non fatal helicopter accidents in the Indian Armed Forces and provides important insight into issues of aero medical interest. Despite the shortcomings in the data, the study provides enough evidence for a reconsideration of the medical standards for helicopter aircrew duties, in particular spinal disabilities.
Keywords
Key words
Injuries
vertebral fractures
helicopter
Despite advancements in the crashworthiness of helicopters, both the rate and severity of injuries sustained in helicopter accidents remain a cause for concern. While various studies have documented the injuries sustained by pilots during ejections [1] and fatal helicopter accidents [2], there has been no analysis of injuries in non fatal helicopter accidents. The mechanism and pattern of injuries sustained in aircraft accidents can provide vital information for improving survivability [3]. Moreover, injury patterns could provide insights into medical standards for helicopter flying duties. There has been no study on the injury patterns in aircrew involved in non fatal helicopter accidents except for a preliminary study involving 12 helicopter aircrew in the Indian Air Force [4]. The present study was carried out to analyze injuries in aircrew involved in non fatal helicopter accidents.
Material and Methods
All aircrew after a helicopter accident are hospitalized for a complete evaluation including full spine roentgenogram. In aircrew, where no spinal injuries are detected on roentgenogram, this is followed by a mandatory MRI within four weeks. If no injuries are detected, aircrew are placed in low medical category for 6 weeks and reviewed at the Institute of Aerospace Medicine at the end of this period before being returned back to flying duties. A case record of each aircrew reporting for evaluation is prepared by the aerospace medicine specialist, which is maintained at the Department of Human Engineering. This record includes report on the clinical examination, radiological findings, results of functional tests and response to simulated aviation stresses. These records were accessed and information for all helicopter aircrew reviewed at the Dept from the years 2000-2006 were included for analysis. Records on a total of 52 aircrew involved in non fatal helicopter accidents during the period of study were retrieved for analysis. Data includes symptomatic as well as asymptomatic aircrew who were downgraded on a strong suspicion of traumatic injury such as PIVD, minimal anterior wedging of the vertebra, spondylolysis, etc. Depending on the clinical and human engineering evaluation, the disposal of these aircrew could range from temporary non-flying, restricted or full flying or even permanent non-flying medical status. Their eventual disposal had no bearing on the inclusion in this study. We categorized military aircrew into two groups - pilot and non-pilot group. In the non-pilot group were included Flight Gunners and Flight Engineers.
Results
Of the 52 aircrew involved in non fatal helicopter accidents, 78.8% were pilots (n= 41) and the remaining non-pilot aircrew (n=l 1) comprised of six Flight Engineers and five Flight Gunners. The mean age of the pilots was 31yrs (24 - 44 yrs) whereas the mean age of the non-pilot aircrew was 33.6 yrs (29 - 49 yrs). All except seven (Army =5, Navy =2) were from the Air Force.
Injuries and type of Helicopter. While large majorities of aircrew were from the Russian origin helicopters, information on the type of helicopter was not available in almost one fourth of the aircrew. Thus no correlation could be made between injury pattern and type of helicopter involved.
Nature of Injuries. The severity of injuries varied from severe fractures to minor lacerations. However, they were all categorized according to the region of the body involved irrespective of its severity. Of the 52 aircrew, there were 7 aircrew (13.5%) who did not suffer any injury. Of the 45 aircrew who suffered some form of injury, 8 had multiple injuries thus giving a total of 53 injuries.
Region-wise distribution of injuries is shown in Fig 1. Of these, 43.4% were spinal injuries (n=23) followed by Head and Face (22.6%, n=12).

- Region-wise distribution of injuries
Spinal injuries. A total of 23 (44.2%) aircrew suffered some form of spinal injuries. Of these, the most common was compression fracture of the vertebra (n=16,69.6%) [Fig 2]. Most of the aircrew had single level vertebral fracture (n=10). A total of 28 vertebral fractures were documented. The highest number of fractures involved the T12 vertebra (n=5) followed by four each at Til and LI. Overall the Tl 1-L1 region accounted for 46.4% of the total vertebral fractures [Fig 3].
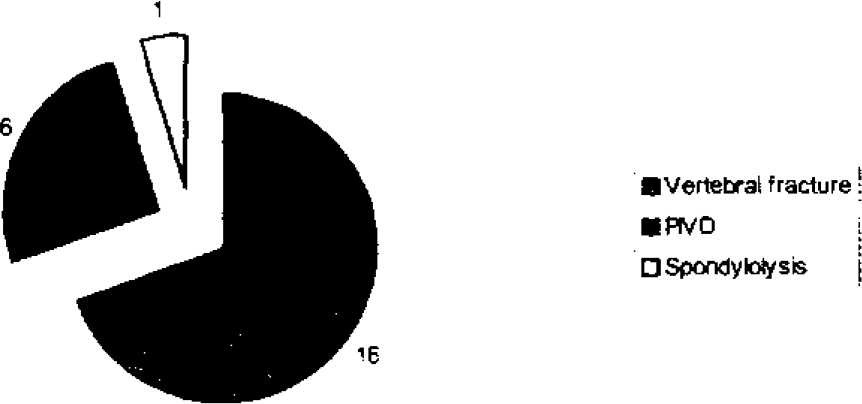
- Nature of spinal injuries in aircrew
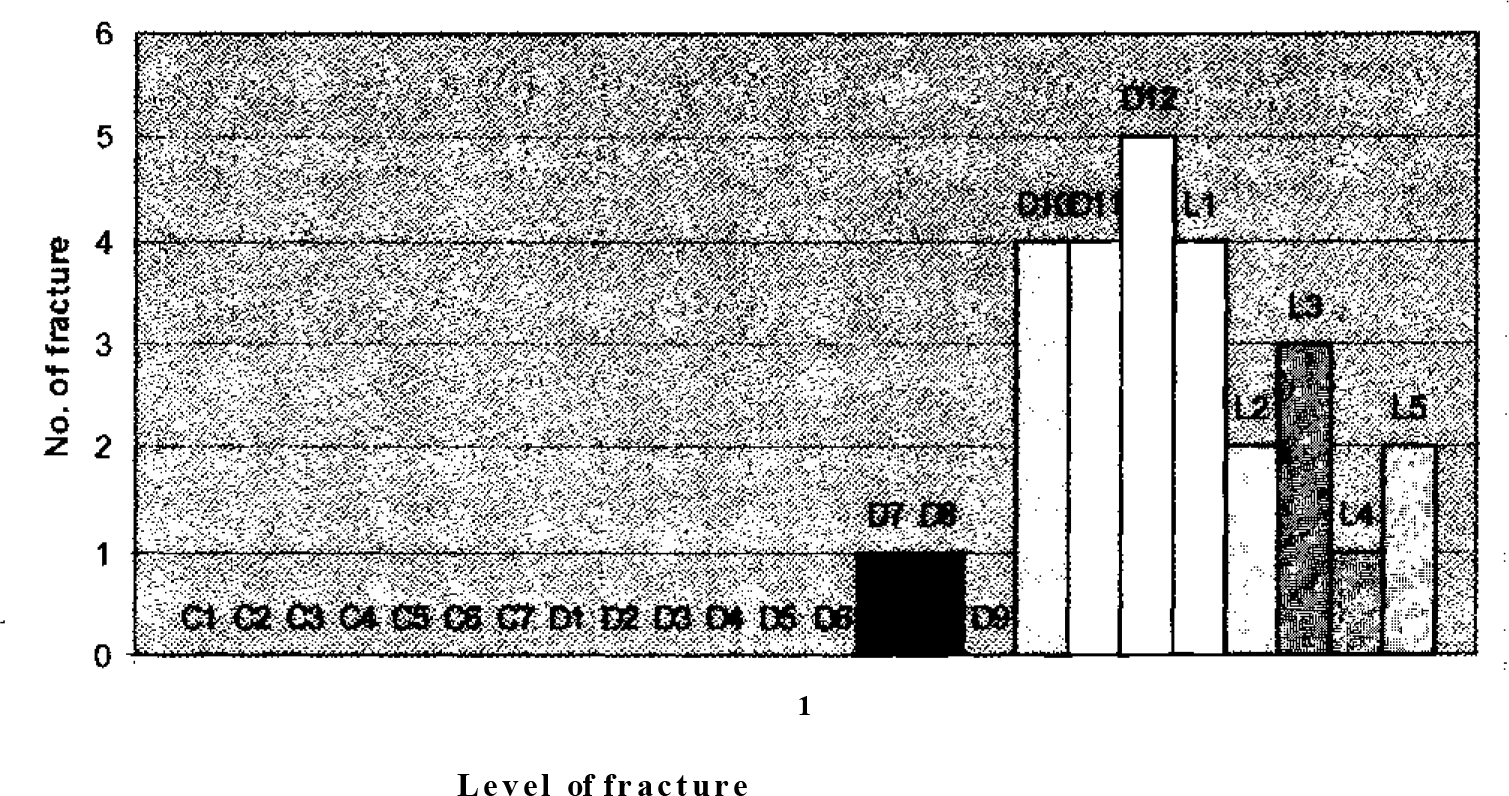
- Distribution of vertebral fractures
The second leading spinal disability was degenerative disc disease detected in six aircrew. The most common site of degenerative disc disease was the C5-6 disc. Two aircrew were initially suspected to have traumatic disc herniation on MRI, but follow up MRIs revealed their non traumatic nature.
Pilot vs Non-pilot aircrew. Differing injury patterns were also evident between pilot and non-pilot aircrew groups as shown in Table 1. The most obvious difference in the injury pattern between pilot and non-pilot aircrew was in the occurrence of spinal and head and face injuries. Of the 11 non-pilot aircrew, only one had a spinal injury compared to 22 pilot aircrew (53.7%) who had spinal injury. On the other hand, non-pilot aircrew suffered higher percentage of head and face injury (fracture/ contusion/laceration) (54.5%) compared to pilots (14.6%).
| Pilot | Non pilot aircrew | |
|---|---|---|
| No. of aircrew | 41 | 11 |
| Multiple injury | 6 | 2 |
| Single injury | 29 | 8 |
| No injury | 6 | 1 |
| Spine | 22 | 1 |
| Head and Face | 6 | |
| Thorax and Shoulder | 3 | 2 |
| Hip and Pelvis | 1 | 0 |
| Upper Limb | 6 | 2 |
| Lower Limb | 3 | 1 |
Discussion
This study provides a preliminary understanding of the nature of injuries in aircrew involved in non fatal helicopter accidents in the Indian Armed Forces and provides important insight into issues of aeromedical interest. They are discussed in the succeeding paragraphs.
(a) Spinal injuries in aircraft accidents. Various studies have suggested that military aircrew may be more prone to develop musculoskeletal disabilities involving the spine compared to non aircrew. Fighter aircrew are believed to be more susceptible to develop disc disease and spinal inuries whereas helicopter aircrew are more likely to develop low backache, spondylolysis and spondylolisthesis [5].
During ejection from fighter aircraft, large Gz forces act in the buttock to head direction in the long axis of the spine. As the line of thrust of the seat and the spinal axis are not parallel, a significant flexion component of this thrust force can lead to large flexion compression of the vertebra during ejection. As a result, the most common type of vertebral fracture seen during ejection is the anterior wedge compression fracture [6].
Spinal injury rates during ejection have varied from a low of 4% to a high of 69% [6]. These differences have been attributed in part to the differences in the type of seat and aircraft. In the Indian Air Force, studies have documented a vertebral fracture rate during ejection from 26.2% to 35.2% (and showing a possible decline with newer generation of ejection seats) [1].
Localization of almost 40-50% of the spinal fractures to the thoracolumbar region is again a characteristic pattern described for ejection injuries [6]. This has been explained by the anatomic-functional characteristics of the thoraco-lumbar junction. This junction acts as a fulcrum between the thoracic kyphosis and lumbar lordosis and owing to its inherent mobility, is particularly subjected to the hyperflexion sustained by the torso during ejection [6].
As is evident, spinal injuries were the leading cause of injuries subsequent to helicopter accidents. Of these, compression fractures constituted more than two- third of all the spinal injuries. This pattern is somewhat similar to spinal injuries during ejection. The distribution of vertebral fractures in helicopter accidents is also strikingly similar to those documented in ejection injuries. Vertebral fractures localised to the thoracolumbar junction (Til-LI) accounted for a little less than half of all vertebral fractures. Our findings corroborate reports of similar injury patterns by Scullion et al [7].
Given the similarities between the magnitude and distribution of spinal injures during ejection and helicopter accidents, it is reasonable to suggest that Gz forces in helicopter accidents and ejection from fighter aircraft might be of similar magnitude leading to compression fracture of vertebra. Further, the acceleration forces during ejection are known as the ejection seats are designed to be within the tolerance limits of human spine. On the other hand, crash forces in helicopter accidents are more likely to be unpredictable and may actually exceed the tolerance limits of the spine leading to a high incidence of spinal injuries among helicopter aircrew [4, 8]. It can be concluded that helicopter aircrew are as susceptible to spinal injuries during accidents, if not more, compared to fighter aircrew
(b) Pilot vs non-pilot aircrew. In this study, the incidence of spinal injuries was found to be significantly low in non-pilot aircrew compared to those in pilots. This may seem to suggest that the non-pilot aircrew were not subjected to high Gz forces along the long axis of spine. Absence of proper seats and restraint system might be the likely explanation for such a difference. On the other hand, the difference in the incidence of head and face injury between pilot and non-pilot aircrew needs further analysis. The non-pilot aircrew do not wear helmets, nor are they restrained by a four five point harness. The consequent flailing into cockpit /aircraft structure due to inadequate restraint may be a plausible explanation, however
(c) Implications for medical fitness for helicopter duties. High occurrence of spinal injuries during helicopter accidents need to be discussed in relation to the spinal abnormalities that are compatible with helicopter flying for in-service candidates. While certain congenital /degenerative spinal disabilities are not compatible with flying duties at entry, they are considered compatible with helicopter and transport aircrew duties when detected in asymptomatic in-service personnel. Some of these disabilities include scoliosis more than 15 degrees as measured by Cobb's method, herniated nucleus pulpous, presence of Schmorl's nodes at more than one level, atlanto-occipital / atlanto-axial anomalies, hemi vertebra and/or-incomplete block (fused) vertebra at any level in cervical, dorsal or lumbar spine, complete block (fused) vertebra at more than one level in cervical or dorsal spine. And unilateral sacralisation or lumbarisation (complete or incomplete) at all levels and bilateral incomplete sacralisation or lumbarisation [9].
The above mentioned disabilities are not considered compatible with fighter flying (ejection seat aircraft) as they may predispose their spine to increased risk of injuries during ejection. Given the high incidence of spinal injuries in pilots involved in non fatal helicopter accidents, with possibly a similar mechanism as spinal injuries during ejection, it is worth debating if these spinal abnormalities should be considered compatible with helicopter flying. Conversely, analysis of helicopter accident databases may reveal that these anomalies did not contribute to worsening of injuries/disability in accidents that resulted in fracture of healthy vertebrae. This kind of information may help determine fitness for fighter flying with some of these anomalies.
(d) Database management and injury scoring systems. There were certain drawbacks in this study, which stem from the inadequate data available for analysis. Comparison of injuries across different helicopters, the type of harness worn at the time of accident, flying hours and injury severity were not documented in most of the records. Towards this, it is suggested that for purposes of standardized data collection, documentation of these variables in each clinical record should be mandatory. Use of injury severity scoring systems will help in categorizing injury so that attention could be focused on severe injuries and not on minor injury, but included with severe injury e.g., laceration scalp included as head injury.
Conclusion
This study is the first attempt of its kind which provides insight into the nature of injuries sustained by aircrew in non fatal helicopter accidents. Despite the shortcomings in the data, the study provides enough evidence for reconsideration of the medical standards for helicopter aircrew duties, in particular spinal disabilities. Recommendations have also been made to revise the data collection process so that more quantifiable and standardized data is available to evaluate the beneficial effects of any future intervention strategies.
References
- Analysis of ejection spinal injuries in IAF (1980-1987) Ind J Aviat Med. 1988;32(1):25-31.
- [Google Scholar]
- Analysis of injuries among pilots killed in fatal helicopter accidents. Aviat Space Environ Med. 2003;74:337-41.
- [Google Scholar]
- Helicopter crash injury: A study of cyclic-related injuries. (Abstract) Aviat Space Env Med. 2002;73(3):242.
- [Google Scholar]
- An analysis of injuries in aircrew involved in non-fatal helicopter accidents: Implications of aircrew medical examination fitness standards. Proceeding of 45 ISAM Conference.
- Spinal injury after ejection in jet pilots: Mechanism, diagnosis, follow-up, and prevention. Aviat Space Environ Med. 1975;46(6):842-848.
- [Google Scholar]
- Injury in U.S. Army helicopter crashes October 1979-September 1985. J Trauma. 1989;29(4):415-22.
- [Google Scholar]






