Translate this page into:
Role of Hyperbaric Oxygen Therapy in Treating A Case of Clostridial Myonecrosis (Gas Gangrene)
Abstract
Clostridial Myonecrosis or Gas Gangrene is an acute, rapidly progressive potentially life threatening Clostridial infection involving the muscles. The preferred treatment is a combination of Hyper Baric Oxygen Therapy (HBOT), surgical debridement of the necrosed tissues and instituting organism specific antibiotics. HBOT acts primarily by eliminating the dangerous alpha toxin produced by the bacilli and reducing oedema and improving perfusion by hyperoxic vasoconstriction. HBOT also enhances phagocytosis which augments the defenses against C perfringens. Here, we discuss a case of Clostridial Myonecrosis (Gas Gangrene), where HBOT was effectively used as an adjunctive treatment with successful outcome.
Keywords
HBOT
Adjunctive Treatment
Clostridial Myonecrosis
Alpha Toxin
Introduction
Clostridial Myonecrosis or Gas Gangrene is an acute, rapidly progressive, non-pyogenic, invasive Clostridial infection involving the muscles. It is characterised by toxaemia, extensive oedema and large scale destruction of tissues [1]. The infection is either an endogenous infection, caused by contamination from a clostridial focus in the body, or an exogenous infection, contracted due to contaminated injuries or medical intervention with unsterilised equipment. This infection is potentially life threatening if not treated empirically and aggressively. The preferred treatment is a combination of Hyper Baric Oxygen Therapy (HBOT), surgical debridement of necrosed tissues and organism specific antibiotics. It is prudent to administer HBOT at the earliest, preferably within 12 hrs to save life and limb of the patient.
Case history
This 28 yr old young civilian male presented with history of fever for which he was administered an intra muscular antipyretic injection in his left gluteal region at a local clinic. Within 24 hours, patient developed severe pain at the injection site for which he went to a tertiary care hospital. On evaluation, the patient was found to have an injection abscess. Incision and Drainage was done with drainage of foul smelling pus. Patient rapidly worsened with decreased urine output, deterioration of renal and hepatic functions associated with increasing cellulitis over left thigh and hip. In view of his worsening condition, surgical debridement was done during which 90% of his Gluteus Maximus (Lt) was found to be necrosed and was debrided. Aerobic culture of the debrided tissue was carried out which showed growth of obligate anaerobic Gram - positive bacilli. Gram stain showed presence of Gram - positive Bacilli morphologically resembling Clostridial species. Diagnosis of Clostridial myonecrosis with sepsis was made. He was managed with antibiotics to which Clostridial infection was sensitive, dialysis for Acute Kidney Injury (AKI) and transfusion with packed cells and platelets to correct anaemia and thrombocytopaenia.
Since there was only a marginal improvement, dialysis was stopped after two days and the case was referred to IAM for Hyperbaric Oxygen Therapy (HBOT) on 11th day since onset. The treatment protocol included HBOT along with surgical debridement/dressings and antibiotics. Daily dose of HBOT was 100% oxygen at 2.5 ATA for a duration of 90 minutes. Positive response was evident on 3rd day of HBOT. The foul smell had reduced substantially with ceasation of myonecrosis. The patient became afebrile and his wound started looking better with appearance of granulation tissue and the clinical progression was good thereafter. By 6th day, wound was healing well with no further spread and the patient was stable enough to be moved from ICU to general surgical ward. Wound swab culture was done which showed no Gram - positive Clostridia. On 7th day due to personal reasons, the patient took ‘Discharge’ from the civil hospital against medical advice and the case was lost to the environment. However, at the time of discharge, he had no fever, wound was healing well, he could move around with support and he resumed normal diet.

- Rapid Recompression Chamber at IAM IAF
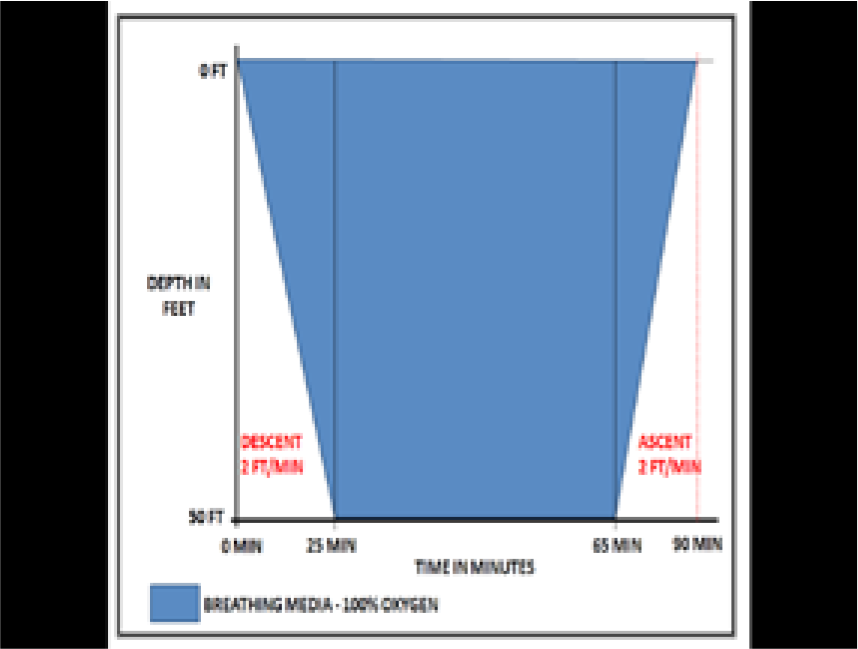
- HBOT Profile
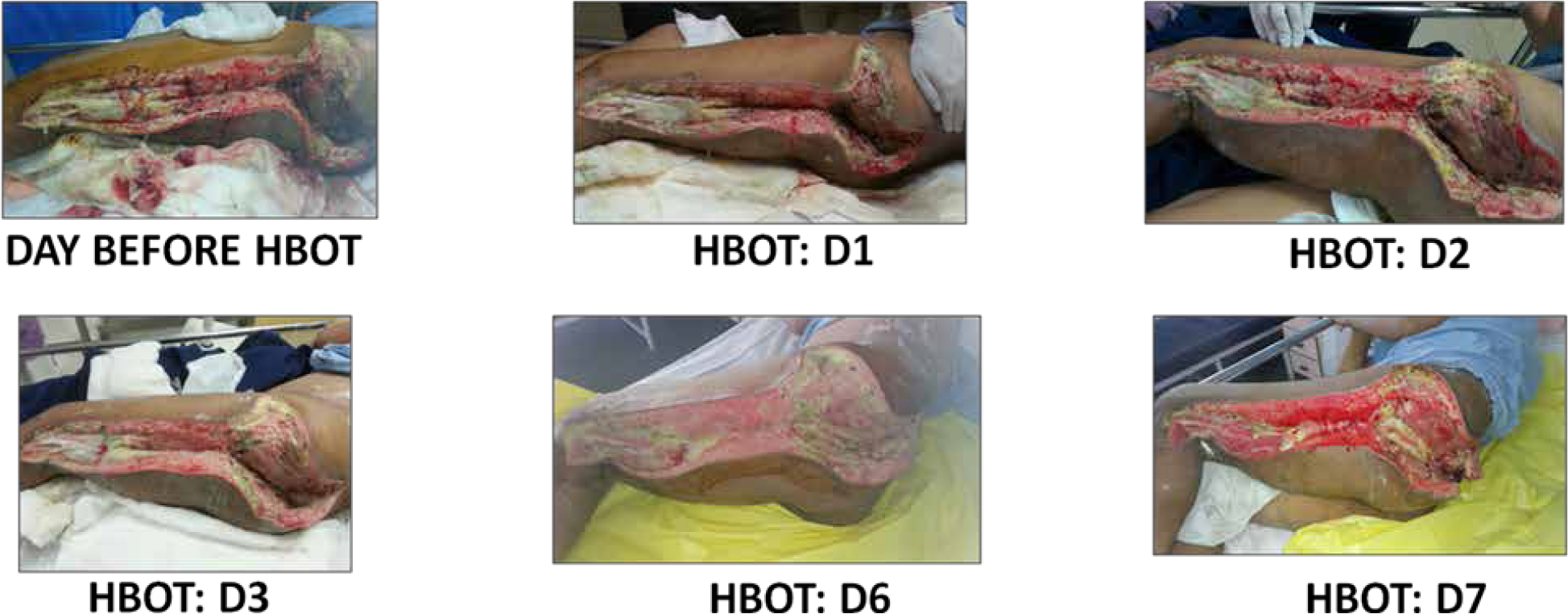
- Serial pictures of effected limb from the day before initiation of HBOT to 7th day of HBOT.
Discussion
Clostridial gas gangrene is a highly lethal necrotizing soft tissue infection of skeletal muscle caused by toxin and gas producing Clostridium species. The synonym Clostridial myonecrosis better describes both the causative agent and the target tissue [1]. The infection is caused by anaerobic, spore forming Gram - positive encapsulated bacilli of the genus Clostridium, discovered by William H. Welch in 1891 [2]. C. perfringens is an anaerobic Gram - positive, rod shaped bacterium formerly referred to as Clostridium welchii. Three organisms responsible for gas gangrene were identified in the late nineteenth century when Pasteur, Welch, and Novy described Clostridium septicum, Clostridium perfringens, and Clostridium novyi, respectively. Six Clostridium species cause gas gangrene in humans, with C. perfringens being the most common. C. perfringens are five types, A–E, distinguished by their individual toxin. There are at least 12 separate toxins produced by this bacterium, and the alpha-type toxin is the most common cause of human gas gangrene [3]. Alpha toxin is hemolytic and tissue necrotising in nature. It destroys platelets and polymorphs and causes wide spread capillary damage, which is often lethal [4]. Gas gangrene develops suddenly with onset occurring between 1 to 6 hours after the injury. It usually occurs at the site of trauma generally a penetrating trauma or a recent surgical wound. Initial symptoms includes seemingly disproportionate pain in a clinically normal area associated with high grade fever. The skin overlying the wound in the early phases appears shiny and tense. Then it becomes dusky and progresses to a bronze discolouration. The infection can advance at a rate of 6 inches per hour. Any delay in diagnosis or initiation of treatment could be fatal. Hemorrhagic bullae or vesicles may also be noted. A thin sero-sanguinolent exudate with a sticky, sweet odour is present. There is gross oedema of the region with wide scale destruction of the soft tissues especially the muscles which appear brown to black or greenish. They are non-contractile areas, which do not bleed when cut. The acute problem in gas gangrene is rapidly advancing infection due to continuous production of alpha toxin in the infected but still viable tissue. If the condition is not treated, the person can go into shock with hypotension, acute kidney injury, sepsis, coma and finally death. Diagnosis of Clostridial myonecrosis is based primarily on clinical suspicion, supported by lab demonstration of Gram - positive rods from the fluids from the effected tissues with virtual absence of leukocytes. The tissue-gas seen on radiographs appears as feather-like figures between muscle fibres and is an early sign and highly characteristic sign of Clostridial myonecrosis. Isolation of the bacilli by culture method confirms the diagnosis [5,6].
Best results in managing such cases of Clostridial myonecrosis are achieved when a three pronged approach is made which includes surgical methods, high dose antibiotics and HBOT. HBOT was first conceived by Brummelkamp and colleagues as treatment modality for anaerobic gas gangrene infections in 1960s [7]. Major retrospective clinical studies done in Europe in mid 80s indicate that the lowest morbidity and mortality are achieved with initial conservative surgery and prompt initiation of HBOT. Results decline progressively when HBOT is delayed. A retrospective clinical study done by Hirn involving 32 cases of gas gangrene showed that mortality and morbidity could be reduced significantly if the disease is recognised early and adequate treatment is instituted in form of operative debridement, antibiotics, HBOT and surgical intensive care [8]. Clostridial myositis and myonecrosis (Gas Gangrene) is an approved indication by Undersea Hyperbaric Medical Society [9].
The action of anaerobe such as Clostridia is based on formation of free radicals in the absence of free-radical degrading enzymes such as dismutase, catalases and peroxidises which have bacteriostatic and bacteriocidal properties. Tissue PaO2 of over 250 mmHg attained during HBOT eliminates the dangerous alpha toxin produced by the bacilli. Because the progressive nature of gas gangrene depends on the continuous production of alpha toxin, hyperbaric oxygen quickly breaks the vicious cycle and shows the benefits [10]. Additional benefits of HBOT include ‘hyperoxic vasoconstriction’ which helps in redusing oedema and increasing perfusion to the ischaemic tissue. Hyperoxia also eliminates the process of acidosis required for toxin production in the adjoining healthy tissue thereby restricting spread of the necrosis. HBOT also enhances phagocytosis which augments the defences against C. perfringens [11].
Conventional use of HBOT for treatment of Clostridial myonecrosis consists of 100% Oxygen at 3.0 ATA pressure for 90 minutes, with 5 minutes air breaks between each 30 minute period of oxygen breathing. The frequency of delivering such treatement is thrice daily on day 1 and twice daily from day 2 to day 5 until the progression of infection appears to have ceased and patient shows resolution of clinical toxicity [6]. HBOT profile given in this particular case at IAM was slightly different from the recommended protocol. The patient was subjected to a common HBOT profile for all medical and surgical conditions which consists of subjecting the patient to pressure of 2.5 ATA for a total of 90 minutes duration. This was done essentially for two reasons, firstly, the patient reported for HBOT on 11th day since onset with slight improvement in general condition but still testing positive for Clostridial infection on culture. Secondly, to see the effectiveness of IAM common profile in managing such conditions. This dose of HBOT was given to the patient continuously for 7 days (including holidays). It was observed that there was significant improvement in clinical condition along with gross reduction in foul smell post 3rd day of HBOT. The wound swab culture carried out on 6th day showed no Gram - positive Clostridia indicating complete resolution of infection.
Role of HBOT as an adjunctive treatment in Clostridial myonecrosis is established. The positive outcome in this case is only proving this fact. However, to prove that the common protocol followed at IAM is appropriate for treating cases of gas-gangrin effectively, needs several clinical trials.
Conclusion
Clostridial Myonecrosis (Gas Gangrene) is a potentially life threatening infection. It can be manage effectively by combination of treatement modalities like surgical debridement/dressings, antibiotics and use of HBOT. The role of HBOT as an adjunctive therapy for treating such infections is already established. Therefore it is recommended all cases of Gas Gangrene must be referred for HBOT as early as possible. The common protocol which is being followed at IAM can also be used for treating cases of Gas Gangrene. But to establish the common protocol is as effective as standard protocol, several clinical trials need to be undertaken in the future.
References
- The pathogenesis of clostridial myonecrosis. Int J Med Microbiol. 2000;290(4-5):497-502.
- [Google Scholar]
- Fulminant massive gas gangrene caused by Clostridium perfringens. Intern Med. 2005;44:499-502.
- [Google Scholar]
- Extremity gas gangrene In: Cameron JL, Cameron AM, eds. Current Surgical Therapy (11th ed). Philadelphia, PA: Elsevier Saunders; 2014. p. :742-45.
- [Google Scholar]
- Hyperbaric oxygen therapy indications: clostridial myonecrosis (gas gangrene) 2008. Hyperbaric oxygen therapy indications [internet]. [cited 2016 Jun 12]; 29-38 Available from: https://www.bayareahyperbarics.com/wp-content/.../uhmsclostridial-myonecrosis.pdf
- [Google Scholar]
- Treatment of anaerobic infections (clostridial myonecrosis) by drenching the tissues with oxygen under high atmospheric pressure. Surgery. 1961;49:299-302.
- [Google Scholar]
- Hyperbaric oxygen in the treatment of gas gangrene and peripheral necrotizing fasciitis: A clinical and experimental study. Eur J Surg. 1993;570(Suppl):9-36.
- [Google Scholar]
- [Internet]. [cited 2016 Mar 23] Available from: https://www.uhms.org/3-clostridialmyositis-and-myonecrosis-gas-gangrene.htmlwww.uhms.org
- [Google Scholar]
- Clostridial myonecrosis In: Oriani G, Marroni A, Wattel F, eds. Handbook of hyperbaric medicine. Milano: Springer; 1996. p. :371-376.
- [Google Scholar]
- Clostridial myositis, necrotizing fascitis and zygomatic infectionsPhysiology and medicine of hyperbaric oxygen therapy Philadelphia: Saunders Elsevier; 2008. p. :402-404.
- [Google Scholar]






