Translate this page into:
Safety in Helicopters: Lessons from the Autopsy Table (An Injury Pattern Analysis of Helicopter Crashes)
Abstract
Background:
Helicopters are essential mode of transportation of men and material to strategically important areas in the northern and the eastern sector of our country. Their unique ability to take off and land vertically without the need of a runway makes them extremely useful tools for military operations, Search and Rescue (SAR) duties and Casualty Evacuation (cas evac). Helicopter accidents impose immense loss to the nation in terms of loss of precious life and costly equipment. Despite most helicopter crashes being relatively low energy impacts, the survivability has remained low due to various factors. This study is a retrospective analysis of data on helicopter crashes in the Indian Armed Forces over the last two decades to evaluate the leading causes of death and most frequently occurring injuries.
Methods:
The data for the study was collected from the air crash archives held with the Department of Aviation Pathology & Toxicology at IAM, IAF Bangalore. Complete data was available for 27 fatal defence helicopter crashes between 1995 to 2015 from IAFF (MS) 1956 records, gross and histopathology reports and photographs of crashes. A total of 74 aircrew fatalities were studied.
Results:
Haemorrhage due to multiple injuries emerged as the commonest cause of death. Head and facial injuries emerged as the most frequent major injuries (23.8%), followed by thoracic (22.2%) and lower limb long bone fractures (18.6%). Spinal injuries, fracture of the pelvis and burns were also common injuries. Mean severity index was calculated for different anatomical regions.
Conclusion:
Injury pattern analysis in fatal helicopter crashes has identified that head & neck is the anatomical region which sustains severe injuries most frequently.
Keywords
Helicopter
Aircraft accidents
Survivability
Preventive strategies
Introduction
Helicopters are essential mode of transportation of men and material to far flung areas which are inaccessible by any other mode of transport. Large areas of strategic importance in the northern and eastern sector of our country are maintained exclusively by the helicopters. Helicopters are used to reach areas that cannot be reached by fixed wing aircrafts. They can land almost anywhere, which makes them useful for military operations, search and rescue, medical evacuations and other high risk missions. With the increasing air traffic, it is imperative to look at the safety issues within these flying machines and improve flight safety. Despite being relatively low energy impacts, survivability in helicopter crashes has been dismal due to a variety of factors. These include presence of overhead rotors, lack of escape/ ejection mechanisms, low flying altitude and proximity of seating to fuel tank etc. In contrast to fighters, the recovery of intact bodies for post-mortem analysis is significantly higher in fatal helicopter crashes. This provides a unique opportunity to study and analyse the pattern of injuries leading to death and devise preventive structural modifications/ strategies.
With the above background, the aim of the study was to determine injuries resulting in mortality in fatal helicopter crashes.
Material & Methods
This was a retrospective analysis of injuries sustained by aircrew in military helicopter crashes from 1995 to 2015. The data was collected from the aircraft accident archives available with the Department of Aviation Pathology & Toxicology at IAM , IAF Bangalore. Only those crashes were included for analysis in which photographic details of the crash site, bodies of victims and helicopters along with gross & histopathological autopsy results were available. Only injuries sustained by aircrew were analyzed as position of aircrew in the helicopter is well defined and likely to remain fixed due to use of harness. Such an analysis provided an evaluation of the effectiveness of safety apparatus used by the aircrew [1]. Fig 1 shows the sequence of analysis of data.

- Sequence of analysis
The following materials were studied to compile the data for analysis:-
IAFF (MS) 1956 (Medical Report on Major Aircraft Accident)
Details of conduct of autopsy
Gross autopsy findings
Histopathological findings on tissues submitted for analysis
Toxicology reports
Available histology slides filed at IAM, IAF Bangalore
Various parameters analyzed were as follows:-
Cause of death
Injuries sustained
Further classification of injuries was based on anatomical region:-
Head & Face
Thorax (Sternum, Ribs, Heart & Lungs)
Upper Limbs
Abdomen & Pelvis (Including Liver & Spleen)
Lower Limbs
Spine
Burns
Severity Index of Injuries. Conversion of injury data from the descriptive autopsy reports to numerical data was achieved by use of numerical scoring based on severity of injuries. Classification of injuries in terms of severity is mentioned in Table 1.
| Severity Index | Nomenclature | Definition |
|---|---|---|
| 1 | Mild | Any minor injury not requiring hospitalization. |
| 2 | Moderate | Any injury requiring hospitalization eg. Single bone fracture/ lacerations/ Burns < 10%, however, not life threatening. |
| 3 | Severe | Multiple fractures/ Head Injury/ Burns 10-50% requiring immediate treatment and possible resuscitation. |
| 4 | Critical | Requiring immediate resuscitation e.g. Multiple long bone fractures/ Fracture of skull & brain Injury/ Rupture of the heart or liver/ Spinal fractures/ Burns >50%. |
| 5 | Fatal | Beyond the limit of Human / Design Tolerance leading to complete disintegration of body |
Severe and Critical Injuries sustained by each anatomical zone were used to calculate “Mean Severity Index” of that zone. The utility of this index is that it incorporates a combined effect of severity and frequency of injuries sustained by an anatomical location and helps in identifying the regions of body receiving most violent force. It also points to a deficiency in safety features designed to provide protection from these forces and need for improvement. To explain the utility of this index, an example is given below:
If Head & Neck of an aircrew has sustained one severe injury and one critical injury, the mean severity index of Head & Neck zone would be (1 x 3 + 1 x 4)/ 2 = 3.5. Similarly, if Thorax has sustained 2 severe and 1 critical injury the mean severity index would be (2 x 3 + 1 x 4)/ 3 = 3.33.
Since the mean severity index of Head & Neck (3.5) is more than that of Thorax (3.3), Head & Neck ranks higher than Thorax in terms of significance for injury potential and need for improvement of safety features.
Multivariate Analysis of Injury Patterns
An attempt was made to analyze the pattern of injuries to identify those injuries which occur together. The hypothesis for this being that grouping of injuries would occur either due to (a) Common hazards/ crash biodynamics or (b) Lack of protective mechanism which can be identified and then mitigated. The analysis was done using a data mining tool called cluster analysis. Cluster analysis is an exploratory data analysis tool which aims at sorting different objects into groups in a way that the degree of association between two objects is maximal if they belong to the same group and minimal otherwise. In this study Agglomerative Hierarchical Cluster Analysis (HCA) was used. At the beginning of the process, each type of injury is in a cluster of its own. The clusters are then sequentially combined into larger clusters until all types of injuries end up being in the same cluster. At each step, two clusters separated by the shortest distance are combined.
Results
Accident Statistics
Helicopter accidents reported (1995 -2015)
Total: 84
Cat I, fatal with complete data and photographs: 27 (32.14%)
Helicopter accident casualties reported:-
Total: 252
-
Fatal (In the 27 crashes analyzed): 117
Aircrew fatalities: 74
Passengers: 43
Salient features of Initial Autopsy Investigations
Complete data from 27 Cat I fatal service helicopter crashes with 74 aircrew fatalities was analyzed. Autopsy was performed in all the cases. Initial autopsy and gross examination of the injuries was conducted by Air Force/ Military pathologists from the nearest Air Force/ Military hospital in 100% cases. In contrast to the fighter and transport crashes, the percentage of availability of preserved bodies for analysis of post mortem remains is significantly higher (>96%) in helicopter crashes. This was one of the reasons for limiting such a study to helicopter crashes. This finding is in contrast to the study of Mathur et al, who had recorded an autopsy rate of 79% in their study [2]. Most autopsies were conducted by Army pathologists in the presence of Aviation Medicine specialist or the unit SMO. In 96% of fatal crashes, bodies of the pilot were strapped on to the seats when recovered.
Cause of Death
Cause of death as recorded in the documents is shown in Fig 2. Hemorrhage due to polytrauma was the commonest cause of death (40.5%). 89.3% of polytrauma cases had fracture of one or more long bones of the lower limbs. Polytrauma was followed by head & neck injuries (24.3%) as the cause of death. All cases of head and neck injuries had two or more fractures of the skull and face (X= 2.45). 90.5% cases of skull or facial bone fractures had lacerations of the brain. Injury to visceral organs like heart, lungs, liver and spleen (20.9%) were the next common causes of death. All cases of visceral injuries were associated with one or more rib fractures. Spinal injuries with or without pelvic injuries were found to be the cause of death in 12.2% cases. Burns were considered as a cause of death in cases where histological evidence of ante-mortem burns was found and burns involved more than 50% of body surface area. Burns as a cause of death were present in 2.1 % causalities in crashes. However, post mortem burns were found in 12.4% fatalities. The findings of the present study were in agreement to those of earlier series [2,3] where too polytrauma was the most commonly reported cause of death.
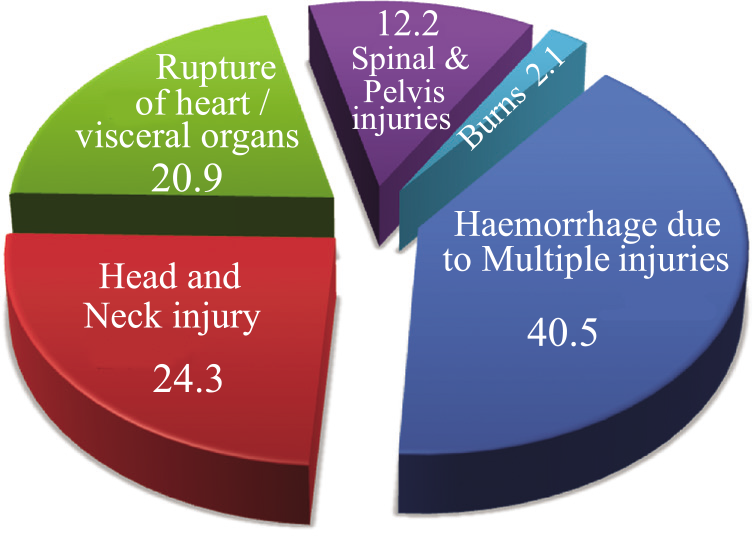
- Cause of death (%)
Gross autopsy findings
The 74 fatal aircrew casualties sustained a total of 483 separate documented injuries. Each aircrew on an average sustained 6.52 injuries. A majority (84%) of these injuries were caused due to impact of the body with surrounding structures or due to severe deceleration. These injuries have been classified according to severity and anatomical region. Details of injury type such as bony, visceral and abrasion, laceration, incised etc have been documented separately but not presented to maintain ease of interpretation of the data. Frequency of injuries according to severity is shown in Table 2.
| Severity index | Nomenclature | Frequency | Percentage |
|---|---|---|---|
| 1 | Mild | 164 | 33.9% |
| 2 | Moderate | 103 | 21.3% |
| 3 | Severe | 114 | 23.7% |
| 4 | Critical | 79 | 16.4% |
| 5 | Fatal | 23 | 4.7% |
| Total | 483 |
Anatomical distribution of all injuries is shown in Fig 3.
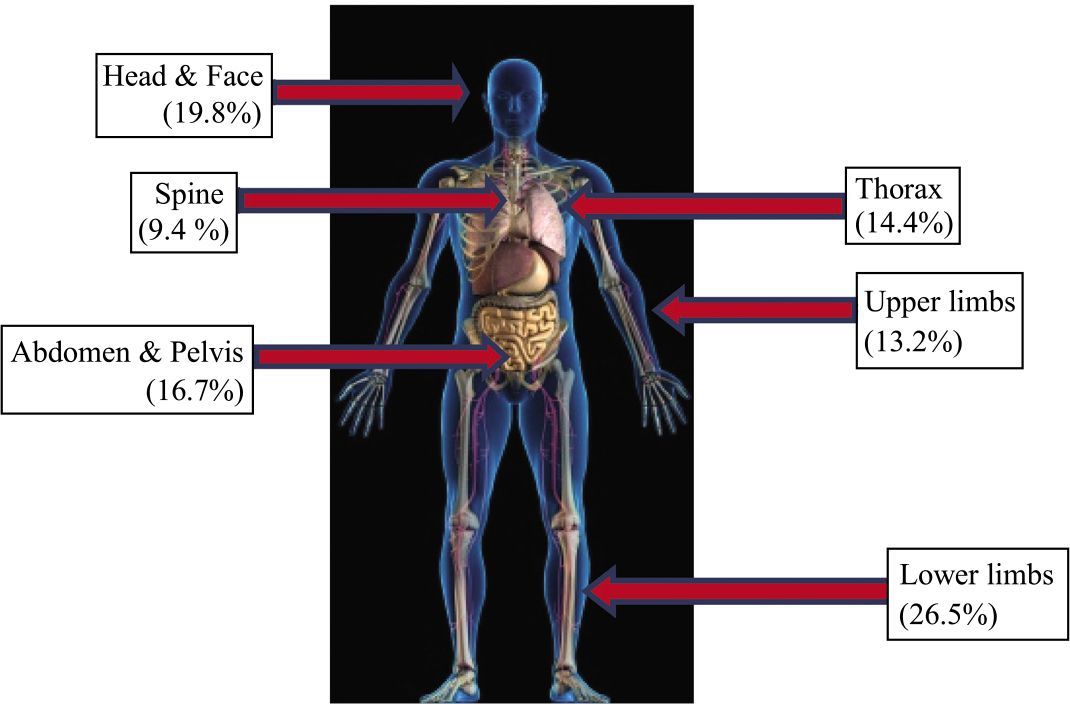
- Frequency of all injuries by location
Severe (Severity Index 3) and critical (Severity Index 4) injuries have been classified into anatomical zones and mean severity index of that region was calculated as shown in Table 3.
| Rank | Zone | Freq | Calculation | Mean Severity Index |
|---|---|---|---|---|
| 1 | Head & Face | 46 (23.8%) | {(15×3)+(31×4)}/46 | 3.67 |
| 2 | Spine | 16 (8.3%) | {(12×3)+ (4×4)}/16 | 3.52 |
| 3 | Thorax | 43 (22.2%) | {(26×3)+(17×4)}/43 | 3.40 |
| 4 | Lower Limbs | 36 (18.7%) | {(24×3)+(12×4)}/36 | 3.33 |
| 5 | Abdomen & Pelvis | 28 (14.5%) | {(20×3)+(8×4}/28 | 3.28 |
| 5 | Burns* | 7 (3.6%) | {(5×3)+ (2×4)}/7 | 3.28 |
| 6 | Upper Limbs | 17 (8.8%) | {(13×3)+(4×4)}/ 17 | 3.23 |
Multivariate analysis of injury patterns
74 fatal aircrew casualties sustained a total of 483 separate documented injuries. Each aircrew on an average sustained 6.52 injuries. Out of these 483 injuries, 248 bony fractures and 41 spinal injuries were documented. Similarly, 86 injuries to visceral organs underlying these fractures were recorded. Table 4 shows step wise clustering carried out on the types of injuries. There are two steps at which we found large change in similarity level and distance level. The first is between step 2 and 3 and the second is between step 5 and 6. Since between step 5 and 6 we find that the total number of cluster entering the model has reached 11, the total number of clusters was fixed at 5.
| Step | Number of clusters | Similarity Level | Distance level | Clusters joined | New Cluster | Number of observations in new cluster | |
|---|---|---|---|---|---|---|---|
| 1 | 11 | 91.7549 | 0.16490 | 1 | 2 | 1 | 2 |
| 2 | 10 | 82.2125 | 0.35575 | 1 | 3 | 1 | 3 |
| 3 | 9 | 72.4493 | 0.55101 | 9 | 10 | 9 | 2 |
| 4 | 8 | 68.2290 | 0.63542 | 11 | 12 | 11 | 2 |
| 5 | 7 | 66.1086 | 0.67783 | 5 | 6 | 5 | 2 |
| 6 | 6 | 57.4651 | 0.85070 | 1 | 9 | 1 | 5 |
| 7 | 5 | 56.9104 | 0.86179 | 4 | 7 | 4 | 2 |
| 8 | 4 | 52.6111 | 0.94778 | 1 | 8 | 1 | 6 |
| 9 | 3 | 48.2625 | 1.03475 | 4 | 11 | 4 | 4 |
| 10 | 2 | 44.9157 | 1.10169 | 4 | 5 | 4 | 6 |
| 11 | 1 | 39.4616 | 1.21077 | 1 | 4 | 1 | 12 |
Table 5 shows clustering of types of injuries in 5 clusters
| Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 |
|---|---|---|---|---|
| Head Injury, Brain laceration, Facial Injuries, Upper Limb, Lower limbs, Pelvic injuries | Spinal injuries, Laceration of liver/ spleen | Chest injuries, Heart laceration | Inhalation of toxic fumes/ Ante mortem Burns | Upper Limb |
Fig 4 is a Dendogram depicting the clustering of types of injuries in 5 clusters. The blue lines show Cluster 1, red lines show cluster 2, green lines show cluster 3, purple lines show cluster 4 and yellow line show cluster 5.
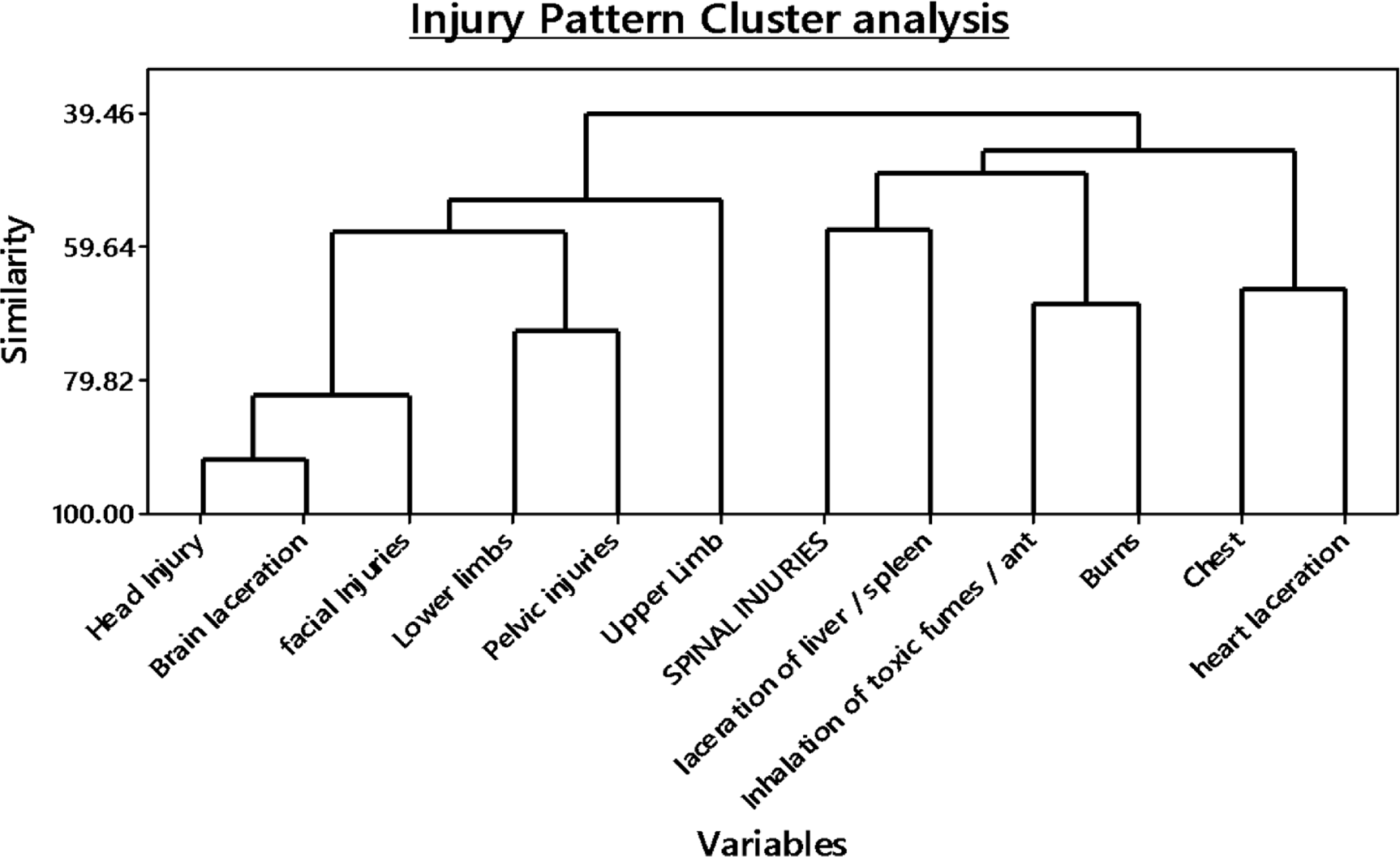
- Dendogram showing the clustering of types of injuries in 5 clusters.The blue lines show Cluster 1, red lines cluster 2, green lines cluster 3, purple lines cluster 4 and yellow line show cluster 5
Salient histological findings
Traumatic Pneumonosis was the commonest histopatho-logical finding and was documented in 84.5% incidents. Mathur et al had reported this incidence to be as high as 92.3% in the aircrew of fighter stream and 75% in aircrew of transport aircraft [2]. Hemorrhage in vital organs was also a common finding in which lungs, liver, heart and spleen were commonly involved. Varying grades of coronary atherosclerosis was observed in 22 out of the 74 cases (29.7%). Histopathological evidence of antemortem burns was found in 7 aircrew and postmortem burns were found in 13 causalities [2,4].
Discussion
The study analyzed all helicopter crashes over two decades 1995-2015. Analysis of 84 crashes was available with the Department of Aviation Pathology & Toxicology, IAM, IAF. However, completed form IAFF (MS) 1956, photographs, whole body X-rays & autopsy reports were available in only 27 crashes (32.14%). Data regarding use of helmet was available in 68% of pilot aircrew only. This points a serious lacuna in reporting of crash data and filling of IAFF (MS) 1956. The findings are similar to the one reported by Sirpal et al and reiterates the need for enhanced awareness and training of the medical officers about filling IAFF (MS) 1956 at the SMCs. Improved reporting of crash data can vastly improve the robustness of studies attempting injury pattern analysis [3].
Recovery of preserved bodies (96.3%) for conduct of autopsy and injury analysis in the present study was significantly higher than that reported by Mathur et al (78%) in fighter crashes. Autopsies were conducted in 100% cases. All autopsies were conducted within 24hrs of recovery of bodies. This is suggestive of good coordination between SMCs and Hospitals. This finding is in contrast to the study by Mathur et al who had recorded an autopsy rate of 79% in their study [2]. Most autopsies were conducted by Army Pathologists in the presence of Aviation Medicine Specialist or the unit SMO. 96% of bodies of the pilot were strapped on to the seats when recovered.
Correlation between injuries sustained by each anatomical region
Cluster 1 shows that injuries are most likely to be caused due to direct trauma to the individual. Of these, it is evident that head injuries are associated closely with brain laceration and facial injuries. Chi square test was carried out to quantify the degree of association and the results are as follows. Head Injury- Brain Laceration (K2 (1) =50.909, p<0.001) and Head injury – Facial Injuries (K2 (1)=30.29, p<0.001). This implies that in fatal helicopter accidents, head injuries along with traumatic brain injury and facial injuries tend to occur together. The unavailability of data in IAFF (MS) 1956 regarding the position and condition/damage of helmets is a drawback in this analysis for drawing further correlations. Such data would have provided information regarding protection provided by the helmet vis-a-vis the impacting force.
Cluster 2 shows that injuries were caused due to decelerative forces at the time of impact with the ground. The clustering shows that spinal injuries tend to be associated with injuries to internal organs such as liver and the spleen. Chi square test for the association of Spinal injuries – injuries to liver and spleen was (K2 (1)=1.394, p=0.33). This shows that the association if at all is not very robust. It is also speculated that there would be additional causes of injury to the abdominal organs due to direct blunt/ penetrative trauma without a spinal injury. This is likely to be a cause for the clustering in multivariate analysis without significant association in the Pearson’s chi square test. What was further interesting to note that spinal injuries do not show statistically significant association with any of the other 10 types of injuries described in this study. This signifies that spinal injuries which may be caused primarily due to decelerative forces may occur without associated traumatic injuries or burns to the individual.
Cluster 3 shows injuries that occurred to the chest and the heart as being a separate group by themselves. Chi square test for the association of chest injuries – laceration of heart was (K2 (1)=7.577, p=0.006). This is to be expected as per the mode of injury. Further, association was also found between chest injuries and the following. chest – lower limbs (K2 (1)=5.139, p=0.023) ; chest – pelvic injuries (K2 (1)=4.464, p=0.035) and lower limb – pelvic injuries (K2 (1)=14.716, p<0.001). The association between chest injuries, lower limb injuries and pelvic injuries suggests a traumatic cause that affects the lower part of the body of the aircrew. In a helicopter cockpit, the Main Instrument Panel (MIP) and the cyclic are likely to be the causative structures. The helicopter is designed to carry out auto-rotation in case there is an emergency on-board. Therefore, the airframe is designed to withstand large decelerative forces in the Gz axis (up – down) however, there is minimal capability in the helicopter to withstand Gx (fore-aft) decelerative forces. Thus, if the helicopter has a high impact angle, the nose of the helicopter gets crushed into the cabin and thus pushes the MIP and the cyclic such that they cause injury to the chest, lower limbs and the pelvis.
Cluster 4 shows injuries caused by burns and due to inhalation of smoke/ fumes ante-mortem by the aircrew. This clustering is to be expected in case of aircraft fire inflight or post-crash. Chi square association for Burn – Inhalation and ante-mortem burns (K2 (1)=9.703, p=0.002). However, the point to note is that there is no significant association of both these modes of injury with any of the other 9 modes of injury. Thus, it can be summarised that on-board/ inflight fire is an independent factor which occurs in a fatal helicopter crash and can be an independent cause of death without associated traumatic or decelerative injuries.
Cluster 5 has injuries to the upper limbs as a single variable in the cluster. Pearson’s Chi Square test for association showed upper limb injuries have no statistically significant association with any other 10 injuries analysed in this study. This finding is explained by the fact that the upper limbs are not restrained and unprotected at the time of a crash. Thus, they are likely to sustain injuries due to flailing and striking cabin structures during impact. Moreover, one of the aircrew is on controls and hence the chances of injury due to direct transmission of crash forces increases chances of injury irrespective of the occurrence of other injuries.
The high incidence of head injuries observed in this study are similar to the findings of multiple US studies. It is estimated that more than 50% fatalities in survivable crashes occur due to head injuries [5]. Smith et al had reported that 62.5 % injuries in all fatal helicopter crashes are head injuries. Most skull fractures are contact or crush injuries due to interaction with the collapsing rotor system or motor assembly overhead. These injuries even when non-fatal severely impair the ability of the occupant to exit the hazardous crash environment. Hence, head injuries deserve the utmost attention to improve crashworthiness and survival [5,6].
Conclusion
This study provides an insight into the nature of injuries sustained in fatal service helicopter crashes. It reinforces the fact that specific contact injuries maybe of greater concern in survivable crashes than deceleration load. Use and further development of restraint systems and helmets can significantly reduce these injuries. Improvement in data collection and reporting can further enhance the strength of such studies. It is proposed that future studies attempting correlation of the crash injuries with the structural hazards in helicopter accidents be carried out to provide vital data which can be used to improve structural design or incorporate safety features which can prevent these injuries.
Limitations of the study
Impact kinematics i.e. speed of impact, angle of impact and ground conditions were not taken into consideration. Differences in the make of helicopter has not been taken into consideration. Lack of complete data of X ray films & reports, copy of COI proceedings not being received at IAM, IAF and details missing from IAFF (MS) 1956 are the other limitations of the study.
References
- An analysis of injuries in fatal aircraft accidents in Indian Air Force. Ind J Aerospace Med. 1988;32(1):32-40.
- [Google Scholar]
- Retrospective analysis of autopsy investigation: Fatal aircraft accidents (1988-1999) Ind J Aerospace Med. 2000;44(2):28-35.5.
- [Google Scholar]
- Analysis of injuries among pilots killed in fatal helicopter accidents. Aviat Space Environ Med. 2003;74:337-41.
- [Google Scholar]
- Aeromedical aspects in air mishap investigation and prevention: The practice in USAF. Ind J Aerospace Med. 2000;44(2):36-41.
- [Google Scholar]
- Injury in U.S. Army helicopter crashes October 1979-September 1985. J Trauma. 1989;29(4):415-22.
- [Google Scholar]
- Fatal occupational injury related to helicopters in United States 1980-1985. Aviat Space Environ Med. 1992;63:67-71.
- [Google Scholar]






